NIAAA Director's Report on Institute Activities to the 132nd Meeting of the National Advisory Council on Alcohol Abuse and Alcoholism
Table of Contents
In Memoriam
Daniel W. Hommer (1948 ― 2013)
Dr. Daniel W. Hommer, M.D., beloved and respected member of the NIAAA research community, served as Chief of the Section of Brain Electrophysiology and Imaging from 1992 until 2012. There Dan led a team of talented researchers who performed groundbreaking work on the structural and functional effects of alcohol on the brain.
Dan, a Fellow of the American College of Neuropsychopharmacology, was world-renowned for his scientific work and inspired many as a both a colleague and friend. He was also widely recognized as one of NIH’s most outstanding mentors in clinical translational research and neuroimaging. Like all great teachers, his greatest legacy will be his students and colleagues whose lives and research he influenced and changed.
Dan will be remembered as a talented scientist whose warmth and generosity touched many.
DIRECTOR'S NOTE
SUAA Update: Future directions and visions of collaboration
As you undoubtedly know, on November 16th NIH Director Dr. Francis Collins announced that after much consideration, NIH had decided to pursue a “functional integration,” of addiction research at NIH, to best serve national research into substance use and addictions. This was one of two options suggested in the SUAA report issued by the Scientific Management and Review Board. The functional reorganization was chosen rather than the other option, a “structural reorganization,” which would have resulted in a new Institute focused on substance use, abuse, and addiction-related research.
“[T]he National Institute on Drug Abuse (NIDA) and the National Institute on Alcohol Abuse and Alcoholism (NIAAA) will retain their institutional identities, while strengthening their ongoing efforts to work more closely with each other and with related research programs at other institutes and centers,” Dr. Collins wrote in a statement announcing his decision.
As Acting Director of NIAAA, I’d like to reiterate that this approach presents extraordinary scientific opportunity. By effectively partnering on specific areas of addictions research with other NIH institutes, our combined efforts are likely to reap greater scientific advances than any of us could achieve alone. At the same time, by retaining NIAAA’s individual focus on alcohol research, we are able to continue to address the unique aspects of alcohol use and its consequences including those aspects of alcohol dependence which differentiate it from other addictions. In short, this arrangement empowers NIH to move addiction-related science forward, making a meaningful impact on a greater number of people’s lives without losing the benefits that accrue from having an institute focused on the effects of alcohol on human health and well-being.
There are many fertile areas for collaboration between NIDA and NIAAA. As highlighted in visions of future partnership, these opportunities include partnering to develop interventions for treating poly-substance addiction and developing combined screening for substance use disorders using mobile and electronic health tools. By pooling resources, we can also strive to conduct clinical trials that more accurately reflect real-world conditions, with greater inclusion of people with multiple addictions and those with comorbid mental health disorders.
By bringing different perspectives and expertise to these cross-cutting areas of research, we have the opportunity to make greater scientific gains. As NIDA and NIAAA join forces, we will be holding joint council meetings. Look to this as an opportunity for cross-fertilization with colleagues, a forum for new perspectives and expertise, and a chance to explore potential areas of synergy. Through our partnership, I am convinced that we can accelerate progress in meeting the needs of our nation as they relate to substance abuse and addiction.
Sincerely,
Ken R. Warren
NIAAA Acting Director
NIAAA BUDGET
FY 2012
In FY 2012, the NIAAA obligated $459.1 million in appropriated money. NIAAA awarded 663 research project grants (RPGs), including 167 competing awards with a success rate of 18.4%. FY 2012 support levels for other key extramural funding mechanisms included 21 research centers for $27.0 million; 133 other research grants for $36.6 million, 287 full-time training positions for $12.0 million; and $40.6 million for research and development contracts.
FY 2013
The NIAAA is currently operating under H.J. Res. 117, a Continuing Resolution (CR) until March 27, 2013. Following the NIH policy under the CR all grants will be funded at 90 percent. This is consistent with NIH practice during the CRs of FY 2006 - 2012. Upward adjustments to awarded levels will be considered after our FY 2013 appropriations are enacted but NIH expects institutions to monitor their expenditures carefully during this period. All legislative mandates that were in effect in FY 2012 remain in effect under the CR, including the salary limitation set at Executive Level II of the Federal Pay Scale ($179,700), which was effective with grant awards with an initial Issue Date on or after December 23, 2011.
FY 2014
The FY 2014 President’s budget request was due to be released on Monday, February 3, but may be delayed.
NIAAA DIRECTOR'S SEARCH
NIH is seeking a permanent Director for the National Institute on Alcohol Abuse and Alcoholism. Applications are being accepted until March 4, 2013.
The Director provides leadership to the Institute and conducts and supports basic, clinical, behavioral research, epidemiological and health services research, research training, and health information dissemination with respect to the treatment of alcohol use disorders. He/she will provide a national focus for the Federal effort to increase knowledge and promote effective strategies to deal with health problems and issues associated with alcohol abuse and alcoholism. To carry out its mission, the NIAAA has a budget of $459 million with staff of over 400 full-time equivalents, contractors, fellows, and trainees…
The full vacancy announcement can be viewed at: http://www.jobs.nih.gov/vacancies/executive/niaaa.htm
DIRECTOR’S ACTIVITIES
| Title of Activity | Date | Director’s Role |
|---|---|---|
| Second European Conference on Fetal Alcohol Spectrum Disorders (FASD) Barcelona, Spain |
October 19-25, 2012 | Plenary Speaker |
| 17th Annual NIAAA Mark Keller Honorary Lecture | November 15, 2012 | Host |
| First National Congress of SIFASD (Italian Society for the FASD) | November 19-22, 2012 | Plenary Speaker |
|
Interagency Coordinating Committee on Fetal Alcohol Spectrum Disorders (ICCFASD) Executive Committee Meeting – NIAAA |
November 29, 2012 | Chair |
| Community Anti-Drug Coalitions of America (CADCA) - 23rd National Leadership Forum | February 5, 2013 | Speaker |
| NIAAA National Advisory Council | February 6-7, 2013 | Chair |
| 3rd International Conference on Applications of Neuroimaging to Alcoholism (ICANA-3) ICANA-3 and Center Directors Meeting |
February 16, 2013 | Speaker |
Upcoming Events
| Title of Activity | Date | Director's Role |
|---|---|---|
| IOM Forum on Neuroscience and Nervous System Disorders | April 8-9, 2013 | Speaker |
| NIAAA Alcohol Research Center Directors Summit Meeting | April 29-30, 2013 | Speaker |
| PASS (Prenatal Alcohol in SIDS and Stillbirth) Network Steering Committee | May 2-3, 2013 | Participant |
| Jack Mendelson, M.D., Honorary Lecture | May 21, 2013 | Host |
STAFF TRANSITIONS
 Dr. Anita Bechtholt-Gompf joined the NIAAA Division of Neuroscience and Behavior as a Program Director in November 2012. In the position, she administers grants related to the effects of ethanol exposure during adolescence on brain structure and function in rodents and humans and also grants relating to comorbid disorders. Prior to joining NIAAA, Dr. Bechtholt-Gompf was a faculty member at Harvard Medical School, where she pursued research on the role of glial cells in the treatments and causes of psychiatric disorders including anxiety, depression, schizophrenia and alcoholism. She completed her post-doctoral training at in the University of Pennsylvania’s School of Medicine and Harvard Medical School - McLean Hospital. Dr. Bechtholt-Gompf earned her Ph.D. in Behavioral Neuroscience from the School of Medicine at Oregon Health & Science University. Her thesis work, supported by NIAAA, examined the role of opioid receptors in specific brain regions in the conditioned rewarding and aversive properties of ethanol.
Dr. Anita Bechtholt-Gompf joined the NIAAA Division of Neuroscience and Behavior as a Program Director in November 2012. In the position, she administers grants related to the effects of ethanol exposure during adolescence on brain structure and function in rodents and humans and also grants relating to comorbid disorders. Prior to joining NIAAA, Dr. Bechtholt-Gompf was a faculty member at Harvard Medical School, where she pursued research on the role of glial cells in the treatments and causes of psychiatric disorders including anxiety, depression, schizophrenia and alcoholism. She completed her post-doctoral training at in the University of Pennsylvania’s School of Medicine and Harvard Medical School - McLean Hospital. Dr. Bechtholt-Gompf earned her Ph.D. in Behavioral Neuroscience from the School of Medicine at Oregon Health & Science University. Her thesis work, supported by NIAAA, examined the role of opioid receptors in specific brain regions in the conditioned rewarding and aversive properties of ethanol.
Fred Donodeo is now serving as Acting Chief of the Communications and Public Liaison Branch. Mr. Donodeo, who joined NIAAA in 1998, has an extensive background in public affairs, social marketing, and community relations. He has been the driving force behind many of NIAAA’s successful outreach efforts, including securing time on Times Square video screens and a series of billboards across the mid-Atlantic region. Other noteworthy projects include seasonal/holiday outreach, sports celebrity youth education projects, NIAAA’s videoconference series, and Congressional briefings.
Mr. Donodeo serves as one of NIAAA's primary representatives to constituent groups, the research community, and the general public. He coordinated the Institute's Task Force on College Drinking, a group comprised of college presidents, scientific researchers, and students, and the current College Presidents Working Group. Before coming to NIAAA, Mr. Donodeo was a Public Affairs Specialist at having joined NIH as a Presidential Management Intern. Prior to that, he managed press and public affairs for the City of New York. Mr. Donodeo has a B.A. in Sociology/Communications from Fordham University and an M.P.A. from George Washington University.
Dr. Yoshihiro Kashiwaya will be returning to his native Japan to practice neurology at Tominaga hospital in Osaka after having spent the last 11 years (and 16 years total) working in the NIAAA Laboratory of Metabolic Control.
STAFF HONORS AND EDITORIAL APPOINTMENTS
Dr. Rui Costa, a guest researcher in the NIAAA Laboratory for Integrative Neuroscience, received the Society for Neuroscience’s Young Investigator Award, given to notable neuroscientists who have received their advanced degree in the past 10 years
Dr. Andrew Holmes, chief of NIAAA’s Laboratory of Behavioral and Genomic Neuroscience was selected as the 2012 recipient of the Jacob P. Waletzky Award from the Society for Neuroscience. The prize is given in recognition of innovative research into substance abuse and the brain and nervous system.
Dr. David Lovinger will become Editor in Chief of the journal Alcohol beginning in 2013.
Dr. John Matochik, Division of Neuroscience and Behavior, received the National Institute of Mental Health Director’s Merit Award from Dr. Tom Insel for his role in scientific management of the Human Connectome Project.
Dr. Pal Pacher was elected as an honorary member of the Hungarian Society for Experimental and Clinical Pharmacology at the International Conference to Celebrate the 50thAnniversary of the Hungarian Society for Experimental and Clinical Pharmacology, September 19-21, 2012. Dr. Pacher was also elected to the Editorial Board of American Journal of Physiology-Cell Physiology.
Dr. Christopher Ramsden will become an Associate Editor of the journal Prostaglandins, Leukotrienes and Essential Fatty Acids beginning in 2013.
NEW RFA’S/PA’S
On October 3, 2012, the NIAAA Division of Neuroscience and Behavior issued a new program announcement (PA) entitled “Epigenetic Inheritance and Transgenerational Effects of Alcohol” (cf. PA-13-003 [R01] and PA-13-004 [R21]). The opening date was January 5, 2013. The program contact is Dr. Matthew Reilly.
On October 25, 2012, the NIAAA Division of Neuroscience and behavior issued a new program announcement entitled “Limited Competition: Brain Tissue Resource Center for Alcohol Research” (cf. PAR-13-011 [R28]). The application due date was January 16, 2013. The program contact is Dr. Matthew Reilly.
On September 28, 2012, the NIAAA Division of Metabolism and Health Effects issued PA-12-291 (R01) and PA-12-292 (R21): “Effects of In Utero Alcohol Exposure on Adult Health and Disease.” The opening date was January 5, 2013 and the program contact is Dr. William Dunty.
Submissions are still being accepted for PA-12-130 (R34): “Pilot Health Services and Economic Research on the Treatment of Drug, Alcohol, and Tobacco Abuse,” which opened May 16, 2012.
NIAAA COMMUNICATIONS & MEDIA COVERAGE
 Seasonal Outreach Series – Projects and Results
Seasonal Outreach Series – Projects and Results
Winter Holidays
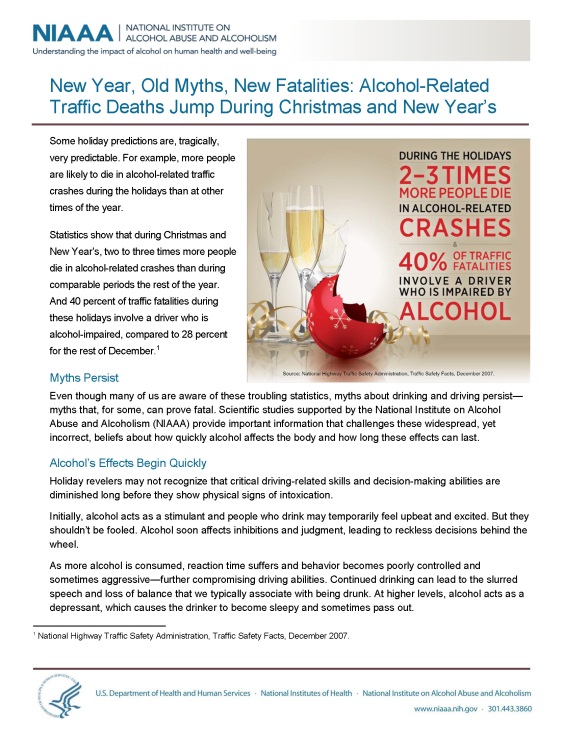
As part of the seasonal outreach around the Christmas and New Year’s holidays, NIAAA used a multipronged approach focusing on traffic fatality statistics (from NHTSA), health messages on moderate drinking, and a link to NIAAA’s Rethinking Drinking website. Expanded efforts this year included:
- The seasonal holiday fact sheet, “New Year, Old Myths, New Fatalities,” was distributed through PR Newswire, generating more than 350 online postings by websites for local TV affiliates, blogs, and news outlets such as the Boston Globe, San Francisco Chronicle, and Sacramento Bee, reaching a total audience of more than 71 million.
- The fact sheet was also distributed by local and national partners such as the Washington Regional Alcohol Program (WRAP), MADD, and the Fairfax County (VA) and Prince George’s County (MD) Police Departments at sobriety checkpoints and special events, and through social media.
- An animated 15-second NIAAA holiday video ran from December 1 to January 3 on the David Letterman screen in New York City’s Times Square, reaching an audience of 1.5 million each day.

- Based on data that indicates increased Interstate traffic during December, we attempted to capture long distance holiday drivers, daily commuters, and suburban drivers traveling into cities for holiday attractions in the mid-Atlantic region, one of the most densely-populated and heavily-traveled areas of the country. NIAAA secured three billboards (Interstate 95 in Baltimore, Philadelphia, and the NJ Turnpike at Newark Airport) with a photo message taken from the fact sheet. Collectively, these billboards reached an audience of more than 1.5 million each week.
- Social Media Outreach: Photo messages were included on NIAAA and NIH websites and in twitter messages, distributed among NIH and liaison community for possible additional placements, and pitched to online food and entertaining media for free placement on their websites.
- 15- second radio PSA, based on content used for video; was pitched to national radio networks; results TBD
- News Media Pitching: Focusing on blackout and hangover themes, and the availability of NIAAA program experts for possible interviews.
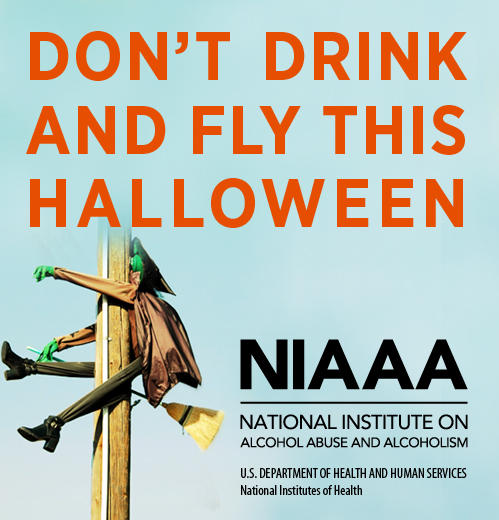

Halloween
As a new addition to its seasonal outreach series, NIAAA disseminated two Halloween-themed “photo messages” for use across digital media to help discourage risky drinking. NIAAA’s goal was to create social media messages that were light-hearted, yet conveyed the seriousness of risky drinking at Halloween. NIAAA promoted the graphics to the liaison community and selected specialty media. Community coalitions, professional associations, and popular media such as People.com (which has 12.3 million unique monthly users and 1 billion average monthly page views) used the graphics as Web banners, Facebook messages, and Twitter messages.
Back to School Outreach
In conjunction with the start of the fall college semester, NIAAA disseminated its fact sheet “Fall Semester: A Time for Parents to Revisit Discussions About College Drinking” through PR Newswire on August 20, 2012. The fact sheet was picked up by 221 media outlets, including Yahoo!, the Boston Globe, the Sacramento Bee, and numerous TV affiliates nationwide, with a total audience of more than 420 million people. In addition, NIAAA developed a 15-second animated billboard incorporating college drinking statistics, which was run on the CBS/David Letterman billboard in New York City’s Times Square.
Positive Website Results from Summer Billboard Pilot
Results on traffic to the Rethinking Drinking website during the summer billboard period were still being calculated when the update was included in the September report. The results are now in, and visits to the website increased 37% from the previous quarter of 2012, and increased 72% when compared to the same quarter of 2011.
NEW MULTI-MEDIA PRODUCTS
New Multi-Media Products
 Alcohol Research: Current Reviews ― Stress and Alcohol
Alcohol Research: Current Reviews ― Stress and Alcohol
The Institute released the latest issue of its peer-reviewed journal on Stress and Alcohol in December. The issue features articles on alcohol and stress in the military, childhood trauma and alcohol dependence, and anxiety and alcohol use disorders, among others. The issue is available at http://pubs.niaaa.nih.gov/publications/arcr344/toc34_4.htm
Alcohol Alert — Stress and Alcohol
In conjunction with the Alcohol Research: Current Reviews issue on stress and alcohol, the Institute released an issue of the Alcohol Alert, summarizing in 8 pages the research findings available in the full journal: http://pubs.niaaa.nih.gov/publications/AA84/AA84.htm
NIAAA News
The winter 2012 issue of the NIAAA News was released in December, featuring a preview of the Institute’s college drinking intervention decision tool and other NIAAA news updates. The issue is available at: http://pubs.niaaa.nih.gov/publications/Newsletter/Winter2012/newsletter_number25.htm
NIAAA Spectrum
NIAAA released the latest issue of the Institute’s online webzine in February. This issue features information on diversity training initiatives at NIAAA and features an interview with Dr. Judy Arroyo, the Institute’s coordinator for minority health and health disparities.
Project MATCH
NIAAA published the Project MATCH Monograph Series over 10 years ago. The initial purpose of this series of manuals was to disseminate methodology developed by the investigators of the multisite clinical trial Project MATCH (1990–1997), an initiative funded by the National Institute on Alcohol Abuse and Alcoholism (NIAAA). Because of the continued interest in the Project MATCH series, NIAAA has repackaged all eight volumes and made them available online for the first time. It is our hope that having this material available in electronic form will make the information even more useful and available to a wider audience. Project MATCH materials are available here: http://pubs.niaaa.nih.gov/publications/ProjectMatch/matchIntro.htm
Press Releases
NIH study finds missed opportunities for underage alcohol screening (January 30, 2013)
Physicians often fail to ask high school-aged patients about alcohol use and to advise young people to reduce or stop drinking, according to a study led by the National Institute on Alcohol Abuse and Alcoholism (NIAAA), part of the National Institutes of Health.
In a random survey of more than 2,500 10th grade students with an average age of 16 years, researchers from NIAAA and the Eunice Kennedy Shriver National Institute of Child Health and Human Development found that 36 percent reported drinking alcohol in the past month. Twenty-eight percent said they had binged, defined as five or more drinks per occasion for males, and four or more for females…
NIH study advances understanding of movement control (January 28, 2013)
Voluntary movements involve the coordinated activation of two brain pathways that connect parts of deep brain structures called the basal ganglia, according to a study in mice by researchers at the National Institute on Alcohol Abuse and Alcoholism (NIAAA), part of the National Institutes of Health. The findings, which challenge the classical view of basal ganglia function, were published online in Nature on Jan. 23.
“By improving our understanding of how the basal ganglia control movements, these findings could aid in the development of treatments for disorders in which these circuits are disrupted, such as Parkinson’s disease, Huntington’s disease and addiction,” says NIAAA Acting Director Kenneth R. Warren, Ph.D.
Heavy Prenatal Alcohol Linked To Childhood Brain Development Problems (October 31, 2012)
Heavy drinking during pregnancy disrupts proper brain development in children and adolescents years after they were exposed to alcohol in the womb, according to a study supported by the National Institutes of Health. The study is the first to track children over several years to examine how heavy exposure to alcohol in utero affects brain growth over time.
Using magnetic resonance imaging (MRI) scans, researchers found that brain growth patterns in children whose mothers drank heavily while pregnant differed from normal patterns of development seen in children who were not exposed to alcohol before birth.
The findings suggest that children with heavy alcohol exposure have decreased brain plasticity – the brain’s ability to grow and remodel itself based on experience with the outside world. Such adaptation continues throughout one’s life and is crucial to learning new skills and adapting to the environment…
Dr. Kenneth Kendler to Deliver 17th Annual Mark Keller Honorary Lecture at NIH (October 13, 2012)
The National Institute on Alcohol Abuse and Alcoholism (NIAAA), part of the National Institutes of Health, announces that Kenneth Kendler, M.D. will deliver the 17th Annual Mark Keller Honorary Lecture. Kendler is a world-renowned expert on the genetics of psychiatric and substance abuse disorders. His presentation is called "The Genetic Epidemiology of Alcohol Use Disorders: A Current Perspective."
NIAAA Researchers Receive Neuroscience Awards (Saturday, October 13, 2012)
Andrew Holmes, Ph.D., chief of the Laboratory of Behavioral and Genomic Neuroscience at the National Institute on Alcohol Abuse and Alcoholism (NIAAA), part of the National Institutes of Health, has been selected as the 2012 recipient of the Jacob P. Waletzky Award from the Society for Neuroscience. The $25,000 prize is given in recognition of innovative research into substance abuse and the brain and nervous system.
Dr. Holmes was presented the honor today at the society’s annual meeting in New Orleans. His work investigates how exposure to stress and the abuse of drugs and alcohol affect cognitive functioning and emotional regulation…
Recent News Media Interviews
Dr. Kenneth Warren was interviewed at the NIH Clinical Center by Felix Kwon of the South Korea Education Broadcasting System, regarding alcohol research. (12/19/12)
Dr. Vivian Faden did a live interview with Marc Sanchez of Minnesota Public Radio on college drinking (12/20/2012).
Dr. Robert Freeman was interviewed by Alison Knopf, Alcoholism & Drug Abuse Weekly, on alcohol and violence (1/23/13).
Dr. Markus Heilig participated in an upcoming segment of SAMHSA’s Road to Recovery TV and Radio series that will explore the inter-relationships of alcohol use disorders, disorders from use of other drugs, and mental disorders.
Dr. Joseph Hibbeln was interviewed by Raj Mukhopadhyay of ASBMB Today (magazine of the American Society for Biochemistry and Molecular Biology) regarding the health effects of omega-3 fatty acids (9/18/12).
Dr. Raouf Kechrid was interviewed by Sonia Sefi of Tunisian National TV for a human interest story about his work at NIAAA (12/13/12).
Dr. Lorenzo Leggio was interviewed by Sonia Gonzalez of Transparences Productions (Paris-based documentary production company), regarding baclofen treatment for alcohol problems (10/26/12).
Dr. Raye Litten was interviewed by Stephanie Booth of Real Simple magazine regarding new treatments for alcoholism (1/28/13).
Dr. Gary Murray was interviewed by:
- Tim Alamenciak, Toronto Star, regarding the health effects of alcohol (1/18/13);
- Jessica Levine of BetterForYou.com on same topic;
- Diana Kelly of Prevention.com on the topic of hangover prevention (12/6/12);
- Sarah Klein of the Huffington Post regarding the brain effects of alcohol (11/27/12);
- Adam Carlson of the CNN.com Health section on hangover treatments (11/26/12);
- Christopher Null of The Daily (San Francisco, CA) regarding the health effects of alcohol (11/7/12);
- Mara Betsch of Discovery Health regarding the health effects of alcohol (9/12/12).
Dr. John C. Umhau was interviewed by Gregg Zoroya of USA Today regarding a study by NIAAA intramural researchers and colleagues at USUHS entitled “Low Vitamin D Status and Suicide: A Case-Control Study of Active Duty Military Service Members,” that appeared in Plos One.
Dr. Aaron White was interviewed by:
- Rachel Pomerance, U.S. News & World Report, regarding the CDC report on women and binge drinking (1/16/13);
- Chris Malina of Wisconsin Public Radio on same topic;
- Christina Vallice of NBC Nightly News on same topic (1/8/13);
- Katie Leslie of the Atlanta Journal-Constitution on the line between social and binge drinking (12/18/12);
- Cathy Clark of the Radio PA State Network, regarding alcohol brain effects and alcohol myths;
- Sarah Klein of the Huffington Post on the brain effects of alcohol (11/27/12);
- Jillian Duchnowski of the Daily Chronicle on alcohol poisoning (12/17/12);
- Tracy Warner of the Fort Wayne Journal Gazette (Indiana) on alcohol poisoning (10/2/12);
- Ellen Hoffman of The Highlander (Misericordia University) on brain effects of teen/young adult binge drinking (11/1/12);
- Rick Docksai of The Futurist magazine regarding alcohol and the teen brain (9/24/12).
Dr. Ellen Witt was interviewed by Rick Docksai of The Futurist magazine, on alcohol and the teen brain (9/24/12).
NOTABLE NIAAA STAFF ACTIVITIES
- Dr. Marcia Scott was the lead on a planning team comprising Drs. Dionne Godette, Mariela Shirley, Kenneth Sher (University of Missouri), and Danielle Dick (Virginia Commonwealth University) in developing the NIAAA-sponsored “Workshop on Establishing a Taxonomy of Alcohol-Related Environmental Exposures on Associated Alcohol Use and Consequences,” that was held on December 6-7, 2012, at NIAAA, and was co-sponsored by the NIH Office of Behavioral and Social Sciences Research (OBSSR). The workshop engaged major researchers in discussions on developing a conceptual approach to examining the role of multi-level ambient, discrete, and cumulative environmental exposures (e.g., chemical, interpersonal, physical and spatial) across a range of alcohol-related outcomes and developmental stages. Presentations from multiple disciplinary perspectives outside of the traditional alcohol field stimulated provocative discussions on research approaches for improving outcomes of future alcohol-related genomic and GxE studies, and informing future programmatic efforts to promote new directions in alcohol research.
- Dr. Judith Arroyo co-chaired and served as discussant for a panel on “Acculturation and Health Risk Behaviors in Hispanic Immigrant Adolescents” at the National Hispanic Science Network in San Diego, CA, September 26-29, 2012. This conference represents a long-standing collaboration between NIAAA and NIDA on minority health issues. NIAAA also sponsored the symposia “Basic and Clinical Evidence of Biomedical Consequences of Alcohol and Drugs of Abuse in HIV/AIDS.” A total of 20 new and established investigators conducting research in alcohol use were supported by NIAAA to disseminate their research at NHSN.
- Drs. Lindsey Grandison and John Matochik co-chaired a symposium at the annual meeting of the Society for Neuroscience on October 13, 2012 in New Orleans. The symposium titled “Prefrontal Cortex-Amygdala Interactions in Control of Behavior” featured investigators from both Europe and the United States describing their cutting-edge advances in this area. The topic of the symposium was also chosen as the Featured Discussion for the week of September 10-16, 2012 for NeurOnLine, the Society for Neuroscience portal for on-line discussions.
- Drs. Soundar Regunathan and Mark Egli organized a satellite symposium entitled “Neural mechanisms of Pain and Alcohol Dependence” at the Society for Neuroscience Annual Meeting in New Orleans on October 13, 2012. The purpose of this satellite symposium was to discuss the current status of research on neurobiological mechanisms influencing pain and alcohol use. The symposium began with the welcome address by Dr. Antonio Noronha, followed by the introduction of the topic, speakers and objectives by Dr. Regunathan. The featured speakers include leading NIAAA funded alcohol investigators, George Koob, Jon Levine and leading pain investigators, Vania Apkarian and Volker Neugebauer. The symposium highlighted brain regions such as the prefrontal cortex, nucleus accumbens and the amygdala that have been demonstrated to play an important role in pain transmission and in the development of alcohol and drug dependence. Another feature of the presentations was the influence of alcohol use on the development of neuropathic pain and chronic pain arising from other sources. The symposium was very well attended with active discussion of the topic. Several important insights and future directions of research were recommended during the discussion. The success of the symposium is further evidenced by the fact that the Editor of the journal Pharmacology, Biochemistry and Behavior has requested a review article on the proceedings of the symposium.
- Dr. Bob Freeman Freeman organized and moderated a NIAAA Workshop titled “Toward Effective Interventions for Alcohol-Related Sexual, Physical, and Intimate Partner Violence: Where We Are, What is Needed, How to Get There,” National Institutes of Health, September 27-28, 2012.
- Dr. Mariela Shirley presented at a forum on NIH Research Priorities and Competitive Grant Writing for Success. Member Services Forum presented to the American Academy of Child and Adolescent Psychiatry, San Francisco, CA, October 25, 2012.
- Mr. Gregory Bloss organized and chaired a teleconference on “Economics of Personalized Health Care and Prevention,” July 19, 2012, and will co-edit a special section of Forum for Health Economics and Policy with several papers that originated in the teleconference. Mr. Bloss also led development and serves as scientific contact for RFA-RM-12-024, “Determinants and Consequences of Personalized Health Care and Prevention (U01),” for which applications are due on February 28, 2013. These activities are part of Mr. Bloss’s work with the NIH Common Fund Health Economics Program.
- Dr. Kathy Jung of the Division of Metabolism and Health Effects gave a presentation entitled “Alcohol modulation of receptor signaling: An overview” in the Alcohol and Immunology Research Interest Group (AIRIG) special symposium on October 27, 2012 at the annual meeting of the Society for Leukocyte Biology in Maui, HI.
- Dr. Raye Litten Organized and Chair session “NIAAA Symposium: Pharmacotherapy of Alcohol Dependence: New Findings,” and presented “Update on Medications Development for Alcohol Treatment,” AAAP Meeting, Aventura, FL, December 6-9 2012.
- Dr. Robert Huebner participated in the 9th Conference for International Network on Brief Interventions for Alcohol and Other Drugs (INEBRIA) September 27-28, 2012 held in Barcelona, Spain. He organized and chaired a symposium entitled “Screening and Brief Intervention for Alcohol Problems in Mental Health Settings: New Findings, New Challenges.” The symposium was well attended and the leadership of the conference was in the audience. He also had in-depth, informal discussions with researchers from Europe, Asia, South America, and the U.S. about possible research collaborations. After the conference, Dr. Huebner met with Dr. Joan Colom, Director of the Program on Substance Abuse to conduct site visits throughout the additional days visiting the Program’s Alcohol Outpatient Unit and Co-Concurring Disorders Unit. These programs are within the program on Substance Abuse, Department of Health of the Government of Catalonia, Barcelona, Spain.
- Dr. Raye Litten served as discussant for session “Opioid and Cannabinoid Mechanisms in Alcohol Addiction: Recent Evidence from Functional Brain Imaging,” ACNP Meeting, Hollywood, FL, December 7-11, 2012.
- Dr. Ralph Hingson presented “Recent Trends and Findings Regarding the Magnitude and Prevention of College Drinking and Drug Use Problems,” at the Clery Center for Security on Campus: Proceeding in Partnership: 25th Anniversary Event, Washington, D.C., October 4, 2012.
- Dr. Ralph Hingson presented “The Science Behind Underage Drinking,” at Mothers Against Drunk Driving’s (MADD) National Conference: Steps to a Safer Nation, Washington, D.C., September 28, 2012.
- Dr. Ralph Hingson presented “Major Substance Abuse Prevention Research Advances in the Past 25 Years,” at the 25th Annual National Prevention Network (NPN) Research Conference, Pittsburgh, PA, September 21, 2012.
NEW AND UPCOMING PUBLICATIONS/MULTI-MEDIA PRODUCTS
Review and Editorial Articles:
Brooks PJ, Zakhari S. Moderate Alcohol Consumption and Breast Cancer in Women: From Epidemiology to Mechanisms and Interventions. Alcohol Clin Exp Res. 2012 Oct 16. Review.
Cui C, Noronha A, Morikawa H, Alvarez VA, Stuber GD, Szumlinski KK, Kash TL, Roberto M, Wilcox MV. New insights on neurobiological mechanisms underlying alcohol addiction. Neuropharmacology. 2012 Nov; S0028-3908(12)00532-1. Review.
Egli M, Koob GF, Edwards S. (2012) Alcohol dependence as a chronic pain disorder. Neuroscience and Biobehavioral Reviews.36(10):2179-92. Review.
Research Articles in Press:
Bertola A, Mathews S, Ki SH, Wang H, Gao B. Mouse chronic plus binge ethanol feeding model (the NIAAA model). Nature Protocols [in press].
White AM, MacInnes E, Hingson RW, Pan IJ. Hospitalizations for suicide-related drug poisonings and co-occurring alcohol overdoses in adolescents (ages 12-17) and young adults (ages 18-24) in the United States, 1999-2008: Results from the Nationwide Inpatient Sample. Suicide and Life-Threatening Behavior [in press].
Books, Book Chapters, and Encyclopedia Entries:
Faden V, Powell P. Epidemiology of Adolescent and Young Adult Alcohol, Tobacco, and Drug Use and Misuse in the United States. Principles of Addiction: Comprehensive Addictive Behaviors and Disorders, Volume I. Miller P. (Ed.). Oxford: Elsevier, Inc. [in press].
Hingson R, White A. Adolescent and Teenage Drinking. Alcohol: Science, Policy, and Public Health. Lowenfels A, Boyle P. (Eds.). Oxford: Oxford University Press [in press].
Hingson R, White A. Costs and Consequences (Morbidity and Mortality) Associated with Adolescent and College Drinking and Related Problems. Principles of Addiction: Comprehensive Addictive Behaviors and Disorders, Volume I. Miller P. (Ed.). Oxford: Elsevier, Inc. [in press].
Hingson R, White A. Prevalence and Consequences of College Student Alcohol Use. College Student Alcohol Abuse: A Guide to Assessment, Intervention, and Prevention. Correia C, Murphy J, Barnett N. (Eds.). Hoboken, NJ: John Wiley & Sons, Inc., 2012.
 Changhai Cui, Lindsey Grandison, and Antonio Noronha are editors for the book on “Neural-Immune Interactions in Brain Function and Alcohol Related Disorders” (ISBN 978-1-4614-4728-3, Springer, 2012, http://www.springer.com/biomed/neuroscience/book/978-1-4614-4728-3).
Changhai Cui, Lindsey Grandison, and Antonio Noronha are editors for the book on “Neural-Immune Interactions in Brain Function and Alcohol Related Disorders” (ISBN 978-1-4614-4728-3, Springer, 2012, http://www.springer.com/biomed/neuroscience/book/978-1-4614-4728-3).
This book integrates emerging knowledge on neural-immune interactions with related key discoveries in alcohol research to provide a comprehensive overview of neuroimmune modulation of brain function and behavior associated with alcohol use disorders. It highlights novel roles of neuroimmune factors in brain function and development, as well as in CNS dysfunctions, including neuroAIDS, neuropsychiatric disorders, and addiction.
WHAT’S AHEAD?
- On May 21, 2013, Dr. Bankole Johnson will deliver a lecture on “Personalizing the Treatment of Alcoholism” at this spring’s Jack Mendelson, M.D., Honorary Lecture. The event will be held 1:30 - 3:30 p.m., in Lipsett Amphitheater at the NIH Clinical Center. Dr. Johnson is chair of the Department of Psychiatry and Neurobehavioral Sciences at the University of Virginia.
- NIAAA has partnered with the NIH Employee Assistance Program to offer free alcohol use disorder screenings on the Bethesda campus during April in recognition of Alcohol Awareness month.
- NIAAA will soon be releasing a publication on available treatment options for alcohol use disorders. This guide is expected to be available in April as well.
- The bi-annual meeting of the Directors of Alcohol Research Centers will be held in New Haven, Connecticut, April 29 and 30, 2013.
NIAAA RESEARCH HIGHLIGHTS
Intramural Research
Concurrent Activation of Striatal Direct and Indirect Pathways During Action Initiation
Voluntary movements involve the coordinated activation of two brain pathways that connect parts of deep brain structures called the basal ganglia, according to a new study in mice conducted by NIAAA researchers. The new findings challenge the classical view of basal ganglia function, which proposes that so-called direct and indirect pathways originating in a brain region called the striatum have opposing effects on movement. Newer models, however, suggest that co-activation of these pathways is necessary to synchronize basal ganglia circuits during movement. By improving understanding of how the basal ganglia control movements, these findings could aid in the development of treatments for disorders in which these circuits are disrupted, such as Parkinson’s disease, Huntington’s disease and addiction.
The basal ganglia are subcortical nuclei that control voluntary actions, and they are affected by a number of debilitating neurological disorders. The prevailing model of basal ganglia function proposes that two orthogonal projection circuits originating from distinct populations of spiny projection neurons (SPNs) in the striatum —the so-called direct and indirect pathways—have opposing effects on movement: activity of direct-pathway SPNs is thought to facilitate movement, whereas activity of indirect-pathway SPNs is presumed to inhibit movement. This model has been difficult to test owing to the lack of methods to selectively measure the activity of direct- and indirect-pathway SPNs in freely moving animals. Here we develop a novel in vivo method to specifically measure direct- and indirect-pathway SPN activity, using Cre-dependent viral expression of the genetically encoded calcium indicator (GECI) GCaMP3 in the dorsal striatum of D1-Cre (direct-pathway-specific) and A2A-Cre (indirect-pathway-specific) mice. Using fibre optics and time-correlated single-photon counting (TCSPC) in mice performing an operant task, we observed transient increases in neural activity in both direct- and indirect-pathway SPNs when animals initiated actions, but not when they were inactive. Concurrent activation of SPNs from both pathways in one hemisphere preceded the initiation of contraversive movements and predicted the occurrence of specific movements within 500 ms. These observations challenge the classical view of basal ganglia function and may have implications for understanding the origin of motor symptoms in basal ganglia disorders. (Cui G, Jun SB, Jin X, Pham MD, Vogel SS, Lovinger DM, Costa RM. Nature. 2013 Jan 23 [Epub ahead of print])
Chronic alcohol remodels prefrontal neurons and disrupts NMDAR-mediated fear extinction encoding
Research suggests that chronic alcohol use may increase the risk for post-traumatic stress disorder (PTSD) by altering the brain’s ability to recover from a traumatic experience. While alcoholism is often linked with PTSD, few studies have explored how chronic drinking may subsequently make a person more prone to such anxiety disorders. In a recent study, NIAAA researchers observed that chronic alcohol exposure altered neurons in the medial prefrontal cortex (mPFC) of mice, making them slower to suppress a conditioned fear response. The results indicate that chronic drinking may impair fear extinction and alter neural circuits that mediate recovery from trauma, increasing the risk for PTSD.
Alcoholism is frequently co-morbid with anxiety disorders, such as post-traumatic stress disorder. Although it is well known that anxiety symptoms occur following a history of heavy drinking, it is not clear how alcohol affects neural circuits mediating the recovery from trauma. Previous studies in rodents have demonstrated that acute or repeated alcohol exposure impairs fear extinction. In this study, Holmes et al. examined the mechanisms underlying the impairment of fear extinction by chronic alcohol exposure. They demonstrated that chronic intermittent ethanol (CIE) exposure down-regulated NMDA receptor expression, altered dendritic morphology, and blunted neuronal encoding of extinction in the medial prefrontal cortex (mPFC). Their findings, for the first time, link the structural and functional changes in the mPFC to alcohol effects on fear extinction. It suggests that chronic alcohol abuse increases the risk of persistent fear by disrupting mPFC function. (Holmes A, Fitzgerald PJ, Macpherson KP, Debrouse L, Colacicco G, Flynn SM, Masneuf S, Pleil KE, Li C, Marcinkiewcz CA, Kash TL, Gunduz-Cinar O, Camp M. Nature Neuroscience. 2012, 15(10):1359-61)
Glucocorticoid receptor dimerization is required for proper recovery of LPS-induced inflammation, sickness behavior and metabolism in mice
Impaired glucocorticoid receptor (GR) function has been associated with impaired metabolic processes, enhanced inflammation and exaggerated sickness and depressive-like behaviors. NIAAA researchers examined the molecular mechanisms underlying GR regulation of physiologic and behavioral responses to a systemic immune challenge. In the study, GR(dim) mice, in which absent GR dimerization leads to impaired GR-DNA-binding-dependent mechanisms but intact GR protein-protein interactions, were administered low-dose lipopolysaccharide (LPS). Their findings indicate that GR dimerization-dependent DNA-binding mechanisms differentially regulate systemic and central cytokine expression in a cytokine- and time-specific manner, and are essential for the proper regulation and recovery of multiple physiologic responses to low-dose endotoxin. The results support the concept that GR protein-protein interactions are not sufficient for glucocorticoids to exert their full anti-inflammatory effects and suggest that glucocorticoid responses limited to GR monomer-mediated transcriptional effects could predispose individuals to prolonged behavioral and metabolic sequelae of an enhanced inflammatory state.
Endogenous glucocorticoids are essential for mobilizing energy resources, restraining inflammatory responses and coordinating behavior to an immune challenge. Impaired glucocorticoid receptor (GR) function has been associated with impaired metabolic processes, enhanced inflammation and exaggerated sickness and depressive-like behaviors. To discern the molecular mechanisms underlying GR regulation of physiologic and behavioral responses to a systemic immune challenge, GR(dim) mice, in which absent GR dimerization leads to impaired GR-DNA-binding-dependent mechanisms but intact GR protein-protein interactions, were administered low-dose lipopolysaccharide (LPS). GR(dim)-LPS mice exhibited elevated and prolonged levels of plasma corticosterone (CORT), interleukin (IL)-6 and IL-10 (but not plasma tumor necrosis factor-α (TNFα)), enhanced early expression of brain TNFα, IL-1β and IL-6 mRNA levels, and impaired later central TNFα mRNA expression. Exaggerated sickness behavior (lethargy, piloerection, ptosis) in the GR(dim)-LPS mice was associated with increased early brain proinflammatory cytokine expression and late plasma CORT levels, but decreased late brain TNFα expression. GR(dim)-LPS mice also exhibited sustained locomotor impairment in the open field, body weight loss and metabolic alterations measured by indirect calorimetry, as well as impaired thermoregulation. Taken together, these data indicate that GR dimerization-dependent DNA-binding mechanisms differentially regulate systemic and central cytokine expression in a cytokine- and time-specific manner, and are essential for the proper regulation and recovery of multiple physiologic responses to low-dose endotoxin. Moreover, these results support the concept that GR protein-protein interactions are not sufficient for glucocorticoids to exert their full anti-inflammatory effects and suggest that glucocorticoid responses limited to GR monomer-mediated transcriptional effects could predispose individuals to prolonged behavioral and metabolic sequelae of an enhanced inflammatory state. (Silverman MN, Mukhopadhyay P, Belyavskaya E, Tonelli LH, Revenis BD, Doran JH, Ballard BE, Tam J, Pacher P, Sternberg EM. Molecular Psychiatry. 2012 Oct 23 [Epub ahead of print])
The rhesus macaque is the most widely used nonhuman primate model organism in biomedical research. Although a draft genome sequence of the rhesus macaque was completed in 2007, there has been no systematic genome-wide comparison of genetic variation of this species to humans. Such studies could inform the macaque’s use as a model for human biology, and could reveal how variation in population history and size alters patterns and levels of sequence variation in primates. In this study, NIAAA researchers sequenced the mRNA transcriptome and specific DNA regions in hippocampus from 14 humans and 14 rhesus macaques. The analyses revealed nearly half a million genetic variants and showed that the macaque has more genetic variation but that its functional variation is not correspondingly expanded. Researchers conclude that the macaque is approximately three times as diverse as the human but more closely equivalent in damaging variation.
As a model organism in biomedicine, the rhesus macaque (Macaca mulatta) is the most widely used nonhuman primate. Although a draft genome sequence was completed in 2007, there has been no systematic genome-wide comparison of genetic variation of this species to humans. Comparative analysis of functional and nonfunctional diversity in this highly abundant and adaptable non-human primate could inform its use as a model for human biology, and could reveal how variation in population history and size alters patterns and levels of sequence variation in primates. We sequenced the mRNA transcriptome and H3K4me3-marked DNA regions in hippocampus from 14 humans and 14 rhesus macaques. Using equivalent methodology and sampling spaces, we identified 462,802 macaque SNPs, most of which were novel and disproportionately located in the functionally important genomic regions we had targeted in the sequencing. At least one SNP was identified in each of 16,797 annotated macaque genes. Accuracy of macaque SNP identification was conservatively estimated to be >90%. Comparative analyses using SNPs equivalently identified in the two species revealed that rhesus macaque has approximately three times higher SNP density and average nucleotide diversity as compared to the human. Based on this level of diversity, the effective population size of the rhesus macaque is approximately 80,000 which contrasts with an effective population size of less than 10,000 for humans. Across five categories of genomic regions, intergenic regions had the highest SNP density and average nucleotide diversity and CDS (coding sequences) the lowest, in both humans and macaques. Although there are more coding SNPs (cSNPs) per individual in macaques than in humans, the ratio of dN/dS is significantly lower in the macaque. Furthermore, the number of damaging nonsynonymous cSNPs (have damaging effects on protein functions from PolyPhen-2 prediction) in the macaque is more closely equivalent to that of the human. This large panel of newly identified macaque SNPs enriched for functionally significant regions considerably expands our knowledge of genetic variation in the rhesus macaque. Comparative analysis reveals that this widespread, highly adaptable species is approximately three times as diverse as the human but more closely equivalent in damaging variation. (Yuan Q, Zhou Z, Lindell SG, Higley JD, Ferguson B, Thompson RC, Lopez JF, Suomi SJ, Baghal B, Baker M, Mash DC, Barr CS, Goldman D. BMC Genetics. 2012 Jun 29;13:52)
Extramural Research
The small g protein h-ras in the mesolimbic system is a molecular gateway to alcohol-seeking and excessive drinking behaviors
Repeated binge or excessive drinking drives the development of alcohol addiction, yet the changes in the brain that contribute to such behavior are unclear. In this study, researchers found that small G-protein H-Ras, a protein primarily involved in regulating cell division, in the nucleus accumbens likely plays a key role in alcohol seeking and excessive drinking behaviors. The scientists found that drinking alcohol activates H-Ras in the nucleus accumbens, a region of the brain that plays a role in reward and pleasure, and that blocking the enzyme with drugs greatly reduced drinking in rats. Similarly, rodents bred to have decreased H-Ras activity showed decreases in alcohol consumption. These findings suggest that H-Ras may be a potential target for treating alcohol use disorders.
Uncontrolled consumption of alcohol is a hallmark of alcohol abuse disorders; however, the central molecular mechanisms underlying excessive alcohol consumption are still unclear. Here, we report that the GTP binding protein, H-Ras in the nucleus accumbens (NAc) plays a key role in neuroadaptations that underlie excessive alcohol-drinking behaviors. Specifically, acute (15 min) systemic administration of alcohol (2.5 g/kg) leads to the activation of H-Ras in the NAc of mice, which is observed even 24 h later. Similarly, rat operant self-administration of alcohol (20%) also results in the activation of H-Ras in the NAc. Using the same procedures, we provide evidence suggesting that the exchange factor GRF1 is upstream of H-Ras activation by alcohol. Importantly, we show that infection of mice NAc with lentivirus expressing a short hairpin RNA that targets the H-Ras gene produces a significant reduction of voluntary consumption of 20% alcohol. In contrast, knockdown of H-Ras in the NAc of mice did not alter water, quinine, and saccharin intake. Furthermore, using two-bottle choice and operant self-administration procedures, we show that inhibiting H-Ras activity by intra-NAc infusion of the farnesyltransferase inhibitor, FTI-276, produced a robust decrease of rats' alcohol drinking; however, sucrose consumption was unaltered. Finally, intra-NAc infusion of FTI-276 also resulted in an attenuation of seeking for alcohol. Together, these results position H-Ras as a central molecular mediator of alcohol's actions within the mesolimbic system and put forward the potential value of the enzyme as a novel target to treat alcohol use disorders. (Ben Hamida S, Neasta J, Lasek AW, Kharazia V, Zou M, Carnicella S, Janak PH, Ron D. Journal of Neuroscience. 2012 Nov 7; 32(45):15849-58)
Resting-state synchrony during early abstinence from alcohol may predict subsequent relapse
The question of why some individuals who stop drinking remain abstinent while others may relapse and resume hazardous drinking is central for the development of strategies to treat alcohol abuse and dependence. The current study sheds light on a possible neural mechanism that may underlie the propensity to relapse. Researchers found that individuals in short-term abstinence (6-15 weeks) that later relapsed had lower resting-state synchrony (correlated activity between certain brain areas during rest) in both the reward and the executive control networks of the brain. This suggests that individuals who may be most likely to relapse have lower functional organization during rest of important brain networks, which could affect impulse control behavior.
Short-term abstinent alcoholics have shown increased engagement of reward regions and reduced engagement of executive control regions. There is no report yet on whether these differences can predict relapse. This is the first study that investigates whether differences in resting-state networks can predict later relapse. Resting-state functional magnetic resonance imaging data were collected from 69 short-term abstinent alcoholics. Participants performed the affective go/no-go task outside of the scanner. At 6-month follow-up, participants were grouped as abstainers (N = 40; age: M = 46.70, standard deviation [SD] = 6.83) and relapsers (N = 29; age: M = 46.91, SD = 7.25). We examined baseline resting-state synchrony (RSS) using seed-based measures. Compared with abstainers, relapsers showed significantly decreased RSS within both the reward and executive control networks as well as within the visual network (P < 0.05). Lower RSS in relapsers could predict relapse (P < 0.05) and was significantly correlated with poor inhibitory control of emotional-laden stimuli (P < 0.017) and with alcohol use (P < 0.05). Results suggest that lower RSS during short-term abstinence may predict subsequent relapse. The association of lower RSS with poorer inhibitory control suggests that low RSS may constitute a faulty foundation for future responses to external cues, which can be manifested as the inability to inhibit behavior. (Camchong J, Stenger A, Fein G. Cerebral Cortex. 2012 July 20 [Epub ahead of print])
Prenatal ethanol exposure stimulates neurogenesis in hypothalamic and limbic peptide systems: Possible mechanism for offspring ethanol overconsumption
New research may shed light on why children exposed to alcohol in the womb have a greater likelihood of developing alcoholism themselves. Similar findings have been observed in animal models, with rodents exposed to alcohol in utero showing increased preference for alcohol. Studying pregnant rats, researchers found that alcohol use during pregnancy altered the development of neurons in the offspring that express certain peptides – small molecules used in neuronal communication – in regions of the brain known to play a role in controlling drinking behavior. The type of peptides involved, called orexigenic peptides, have been shown to stimulate drinking in adult animals.
Exposure to ethanol during the prenatal period contributes to increased alcohol consumption and preference in rodents and increased risk for alcoholism in humans. With studies in adult animals showing the orexigenic peptides, enkephalin (ENK), galanin (GAL) and orexin (OX), to stimulate ethanol consumption, the question addressed here is whether prenatal ethanol alters the development in utero of specific neurons that express these peptides. With reports describing suppressive effects of high doses of ethanol, we examined the offspring of dams gavaged from embryonic day 9 to parturition with a control solution or lower ethanol doses, 1 and 3g/kg/day, known to promote ethanol consumption in the offspring. To understand underlying mechanisms, measurements were taken in postnatal offspring of the expression of ENK in the hypothalamic paraventricular nucleus (PVN) and nucleus accumbens (NAc), GAL in the PVN, and OX in the perifornical lateral hypothalamus (PFLH) using real-time qPCR and in situ hybridization, and also of the cell proliferation marker, 5-bromo-2-deoxyuridine (BrdU), and its double-labeling with either neuronal nuclei (NeuN), a marker of mature neurons, or the peptides. On postnatal day 15 (P15), after two weeks without ethanol, the offspring showed increased expression of ENK in the PVN and NAc core but not shell, GAL in the PVN, and OX in the PFLH. In these same areas, prenatal ethanol compared to control increased the density at birth (P0) of neurons expressing these peptides and at P0 and P15 of neurons double-labeling BrdU and NeuN, indicating increased neurogenesis. These BrdU-positive neurons were found to express ENK, GAL and OX, indicating that prenatal ethanol promotes neurogenesis in these specific peptide systems. There were no changes in gliogenesis or apoptosis. This increase in neurogenesis and density of peptide-expressing neurons suggests the involvement of these hypothalamic and accumbal peptide systems in mediating the increased alcohol consumption observed in prenatal ethanol-exposed offspring. (Chang GQ, Karatayev O, Liang SC, Barson JR, Leibowitz SF. Neuroscience. 2012 Oct 1;222:417-28)
2012 Oct 11; 222:417-28). 2012 Oct 11; 222:417-28).2012 Oct 11; 222:417-28).2012 Oct 11; 222:417-28).
Ethanol disrupts axon outgrowth stimulated by netrin-1, GDNF, and L1 by blocking their convergent activation of Src family kinase signaling
Drinking alcohol during pregnancy can cause fetal alcohol spectrum disorders (FASD), the most common preventable cause of developmental disability. The developing cerebellum is particularly vulnerable to the effects of alcohol. NIAAA-supported researchers have previously reported that alcohol inhibits the stimulation of axon outgrowth in cerebellar granule neurons (CGN), the most common type of neuron in the brain. In the current study, researchers used CGN to demonstrate that axon outgrowth in these cells stimulated by the growth factors L1, netrin-1, and GDNF depend on the activation of a Src family kinase (SRK), and that these processes were inhibited by alcohol. In contrast, BDNF-induced outgrowth was found to be SRK-independent and insensitive to alcohol. These findings indicate that SRK-mediated mechanisms of axon outgrowth are specifically impaired by alcohol and that the relevant SRK or an upstream component involved in its activation may be a direct target of alcohol. These mechanistic insights may inform the development of FASD interventions.
Pre-natal alcohol exposure causes fetal alcohol spectrum disorders (FASD), the most common, preventable cause of developmental disability. The developing cerebellum is particularly vulnerable to the effects of ethanol. We reported that ethanol inhibits the stimulation of axon outgrowth in cerebellar granule neurons (CGN) by NAP, an active motif of activity-dependent neuroprotective protein (ADNP), by blocking NAP activation of Fyn kinase and its downstream signaling molecule, the scaffolding protein Cas. Here, we asked whether ethanol inhibits the stimulation of axon outgrowth by diverse axon guidance molecules through a common action on the Src family kinases (SFK). We first demonstrated that netrin-1, glial cell line-derived neurotrophic factor (GDNF), and neural cell adhesion molecule L1 stimulate axon outgrowth in CGNs by activating SFK, Cas, and extracellular signal-regulated kinase 1 and 2 (ERK1/2). The specific SFK inhibitor, PP2, blocked the stimulation of axon outgrowth and the activation of the SFK-Cas-ERK1/2 signaling pathway by each of these axon-guidance molecules. In contrast, brain-derived neurotrophic factor (BDNF) stimulated axon outgrowth and activated ERK1/2 without first activating SFK or Cas. Clinically relevant concentrations of ethanol inhibited axon outgrowth and the activation of the SFK-Cas-ERK1/2 pathway by netrin-1, GDNF, and L1, but did not disrupt BDNF-induced axon outgrowth or ERK1/2 activation. These results indicate that SFK, but not ERK1/2, is a primary target for ethanol inhibition of axon outgrowth. The ability of ethanol to block the convergent activation of the SFK-Cas-ERK1/2 pathway by netrin-1, GDNF, L1, and ADNP could contribute significantly to the pathogenesis of FASD. (Chen S, Charness ME. Journal of Neurochemistry. 2012 Nov;123(4):602-12, 2012)
Drinking context and intimate partner violence: evidence from the California community health study of couples
This is the first study to examine associations between male and female partner’s drinking in
various contexts and the risk for intimate partner violence in the past year in a sample of married/cohabiting couples. The researchers found that some of the hypothesized associations were observed; for example, drinking volume in particular locations or contexts, such as bars, parties, and parks and public places, was associated with elevated risk for partner violence after taking into account the frequency of intoxication and other demographic and psychosocial IPV risk factors. Most of these associations, however, were significant for the male partner only. The findings suggest that environmental factors, especially certain settings in which the male partner drinks, confer additional risk for IPV perpetration and victimization and need to be considered within the framework of the couple’s interactions and characteristics. These results point to the importance of considering not just the amount of alcohol consumed but also the context of drinking in relation to violent and aggressive behavior.
Couples in which one or both partners is a heavy or problem drinker are at elevated risk for intimate partner violence (IPV), yet little is known about the extent to which each partner's drinking in different contexts (volume consumed per setting in bars, parties, at home, or in public places) increases the likelihood that partner aggression will occur. This study examined associations between the volume consumed in different settings by each partner and the occurrence and frequency of IPV. We obtained a geographic sample of married or cohabiting couples residing in 50 medium to large California cities. Cross-sectional survey data were collected via confidential telephone interviews (60% response rate). Logistic and negative binomial regression analyses were based on 1,585 couples who provided information about past-12-month IPV, drinking contexts (number of times attended, proportion of drinking occasions when attended, average number of drinks), frequency of intoxication, and psychosocial and demographic factors. Drinking context-IPV associations for each partner were adjusted for the other partner's volume for that context and other covariates. Male partner's volume per setting for bars and parks or public places was associated with the occurrence and frequency of male-to-female IPV and female-to-male IPV. Male's volume per setting for quiet evening at home was associated with the occurrence of female-to-male IPV; female partner's volume for this setting was associated with the frequency of male-to-female IPV and female-to-male IPV. Among couples in the general population, each partner's drinking in certain contexts is an independent risk factor for the occurrence and frequency of partner aggression. (Cunradi CB, Mair C, Todd M, Remer L. Journal of Studies on Alcohol and Drugs. 2012 Sep;73(5):731-9)
Alcohol Consumption as a Barrier to Prior HIV Testing in a Population-Based Study in Rural Uganda
Previous research has shown that alcohol abuse negatively affects adherence to HIV medications and overall progression of the disease. For the first time, investigators have shown that alcohol use also adversely affects HIV testing in women, a critical step in the early treatment of HIV/AIDS. A study of 2,500 men and women in Uganda revealed that women who currently drank heavily and those who reported drinking alcohol in the past 1 to 5 years were less likely to have been tested for HIV. Alcohol use showed no relationship to HIV testing in men. These findings suggest that targeting women who drink alcohol for HIV testing could be an important part of strategies to combat HIV/AIDS.
Early receipt of HIV care and ART is essential for improving treatment outcomes, but is dependent first upon HIV testing. Heavy alcohol consumption is common in sub-Saharan Africa, a barrier to ART adherence, and a potential barrier to HIV care. We conducted a population-based study of 2,516 adults in southwestern Uganda from November-December 2007, and estimated the relative risk of having never been tested for HIV using sex-stratified Poisson models. More men (63.9 %) than women (56.9 %) had never been tested. In multivariable analysis, compared to women who had not consumed alcohol for at least 5 years, women who were current heavy drinkers and women who last drank alcohol 1-5 years prior, were more likely to have never been tested. Alcohol use was not associated with prior HIV testing among men. HIV testing strategies may thus need to specifically target women who drink alcohol. (Fatch R, Bellows B, Bagenda F, Mulogo E, Weiser S, Hahn JA. AIDS and Behavior. 2012 Aug 10. [Epub ahead of print])
A Typology of Violence Against Self and Others and Its Associations With Drinking and Other Drug Use Among High School Students in a U.S. General Population Survey
Students who use drugs or alcohol are more likely to have engaged in violent behavior over the past year, based on findings from an NIAAA study. Researchers analyzed responses from more than 43,000 high school students in the U.S. and found that about one in four (24%) reported some form of violence – 17% reported violence directed at another person, 4.2% said their violence was self-directed, and 2.9% reported violence that was both self-directed and directed at others. Students in this combined violence category had the greatest levels of drug and alcohol use and self-reported depression. The study also suggests that the risk for violence against others and combined violent behavior increases with the frequency of binge drinking. While previous studies have identified binge drinking as a strong risk factor for suicidal behavior, the current study found that binge drinking and marijuana use are more likely to be linked to other-directed than to self-directed violence.
This study examines associations between binge drinking and other substance use and perpetration of violence against self and others. Data were pooled from the 2003, 2005, and 2007 Youth Risk Behavior Surveys, yielding a sample of 43,172 U.S. high school students. A typology was constructed to reflect four categories of behaviors: other-directed violence only, self-directed violence only, combined other- and self-directed violence, and no violence. Results from multinomial logistic regressions show that the frequency of binge drinking and other substance use were significant risk factors for each of the violence categories relative to no violence. However, the strengths of these associations varied across the violence categories. (Harford TC, Yi H-y, Freeman RC. Journal of Child & Adolescent Substance Abuse. 2012 Sept-Oct;21(4):349-366)
Physician Advice to Adolescents About Drinking and other Health Behaviors
Physicians often fail to ask high school-aged patients about alcohol use and to advise young people to reduce or stop drinking, according to a study led by the NIAAA. A random survey of more than 2,500 10th grade students found that 36 percent reported drinking alcohol in the past month, and 28 percent said they had binged, defined as five or more drinks per occasion for males, and four or more for females. Although more than 80 percent of 10th graders said they had seen a doctor in the past year, just 54 percent of that group were asked about drinking, and 40 percent were advised about alcohol harms. Among students who had been seen by a doctor in the past year and who reported drinking in the past month, only 23 percent said they were advised to reduce or stop drinking. The findings indicate a need for stronger efforts to help clinicians make alcohol screening a routine part of patient care for young people.
This report assessed the proportion of US 10th graders (average age, 16) who saw a physician in the past year and were asked and given advice about their drinking. We hypothesized that advice would vary by whether students were asked about drinking and their drinking, bingeing, and drunkenness frequency. A nationally representative sample of 10th graders in 2010 (N = 2519) were asked their past 30-day frequency of drinking, bingeing, and intoxication and whether, during their last medical examination, their drinking was explored and they received advice about alcohol’s risks and reducing or stopping. In the past month, 36% reported drinking, 28% reported bingeing, and 23% reported drunkenness (11%, 5%, and 7%, respectively, 6 or more times). In the past year, 82% saw a doctor. Of that group, 54% were asked about drinking, 40% were advised about related harms, and 17% were advised to reduce or stop. Proportions seeing a doctor and asked about drinking were similar across drinking patterns. Respondents asked about drinking were more often advised to reduce or stop. Frequent drinkers, bingers, and those drunk were more often advised to reduce or stop. Nonetheless, only 25% of them received that advice from physicians. In comparison, 36% of frequent smokers, 27% of frequent marijuana users, and 42% of frequent other drug users were advised to reduce or quit those behaviors. Efforts are warranted to increase the proportion of physicians who follow professional guidelines to screen and counsel adolescents about unhealthy alcohol use and other behaviors that pose health risks. (Hingson R, Zha W, Iannotti RJ, Simons-Morton B. Pediatrics. 2013 Jan 28. [Epub ahead of print])
HSPB2 is dispensable for the cardiac hypertrophic response but reduces mitochondrial energetics following pressure overload in mice
The small heat shock proteins (sHSPs) are expressed in virtually all organisms, from bacteria to humans. Scientists believe sHSPs play tissue-specific and specialized roles, and the nature of these functions is under active investigation. In the current study, NIAAA scientists describe a new mouse model characterized by the cardiac-specific deletion of the hspb2 gene (HSPB2cKO). Under normal conditions, HSPB2cKO did not exhibit any obvious cardiac abnormality. They further demonstrated that lack of HSPB2 did not modify the cardiac response to pressure overload in response to either mild or severe stress. The findings indicate that HSPB2 can be replaced by other members of the multigene small HSP family under basal conditions while HSPB2 is implicated in the regulation of metabolic/mitochondrial function under cardiac stress. The new mouse model provides a valuable tool to further investigations of additional roles of HSPB2.
CryAB (HspB5) and HspB2, two small heat shock genes located adjacently in the vertebrate genome, are hypothesized to play distinct roles. Mice lacking both cryab and hspb2 (DKO) are viable and exhibit adult-onset degeneration of skeletal muscle but confounding results from independent groups were reported for cardiac responses to different stressful conditions (i.e., ischemia/reperfusion or pressure overload). To determine the specific requirements of HSPB2 in heart, we generated cardiac-specific HSPB2 deficient (HSPB2cKO) mice and examined their cardiac function under basal conditions and following cardiac pressure overload. Transverse aortic constriction (TAC) or sham surgery was performed in HSPB2cKO mice and their littermates (HSPB2wt mice). Eight weeks after TAC, we found that expression of several small HSPs (HSPB2, 5, 6) was not markedly modified in HSPB2wt mice. Both cardiac function and the hypertrophic response remained similar in HSPB2cKO and HSPB2wt hearts. In addition, mitochondrial respiration and ATP production assays demonstrated that the absence of HSPB2 did not change mitochondrial metabolism in basal conditions. However, fatty acid supported state 3 respiration rate (ADP stimulated) in TAC operated HSPB2cKO hearts was significantly reduced in compared with TAC operated HSPB2wt mice (10.5±2.2 vs. 12.8±2.5 nmol O(2)/min/mg dry fiber weight, P<0.05), and ATP production in HSPB2cKO hearts was significantly reduced in TAC compared with sham operated mice (29.8±0.2 vs. 21.1±1.8 nmol ATP/min/mg dry fiber weight, P<0.05). Although HSPB2 was not associated with mitochondria under cardiac stress, absence of HSPB2 led to changes in transcript levels of several metabolic and mitochondrial regulator genes. The present study indicates that HSPB2 can be replaced by other members of the multigene small HSP family under basal conditions while HSPB2 is implicated in the regulation of metabolic/mitochondrial function under cardiac stress such pressure overload. (Ishiwata T, Orosz A, Wang X, Mustafi SB, Pratt GW, Christians ES, Boudina S, Abel ED, Benjamin IJ. PLoS One. 2012 Aug 1;7(8):e42118)
Family-based genome-wide association study of frontal theta oscillations identifies potassium channel gene KCNJ6
Event-related oscillations (EROs) are highly heritable neuroelectric correlates of cognitive deficits in alcoholics and in children at high risk to develop alcoholism. For example, theta ERO to targets in the visual oddball task – in which subjects are instructed to detect infrequently occurring target sensory stimuli imbedded in an otherwise repetitive train of frequent standard stimuli -- has been shown to be a biological marker for alcoholism. In the current study, researchers genotyped 1560 family members from 117 families densely affected by alcohol use disorders and then determined if specific genetic variants were associated with the theta ERO marker. Their findings indicate that variants in the potassium channel gene KCNJ6 or its product account for some of the variations in frontal theta band oscillations.
Event-related oscillations (EROs) represent highly heritable neuroelectric correlates of cognitive processes that manifest deficits in alcoholics and in offspring at high risk to develop alcoholism. Theta ERO to targets in the visual oddball task has been shown to be an endophenotype for alcoholism. The authors genotyped 1560 family members (using single nucleotide polymorphisms or SNPs) from 117 families densely affected by alcohol use disorders, recruited in the Collaborative Study on the Genetics of Alcoholism. A family-based genome wide association study was performed for the frontal theta ERO phenotype. Genome-wide significant association was found with several SNPs on chromosome 21 in KCNJ6 (a potassium inward rectifier channel; KIR3.2/GIRK2), with the most significant SNP at P = 4.7 × 10−10. These results suggest KCNJ6 or its product GIRK2 account for some of the variations in frontal theta band oscillations. GIRK2 receptor activation contributes to slow inhibitory postsynaptic potentials that modulate neuronal excitability, and therefore influence neuronal networks. (Kang SJ, Rangaswamy M, Manz N, Wang JC, Wetherill L, Hinrichs T, Almasy L, Brooks A, Chorlian DB, Dick D, Hesselbrock V, Kramer J, Kuperman S, Nurnberger J Jr, Rice J, Schuckit M, Tischfield J, Bierut LJ, Edenberg HJ, Goate A, Foroud T, Porjesz B. Genes, Brain and Behavior. 2012 Aug;11(6):712-9)
This study is one of the first to investigate epigenetic changes in living neurons derived from psychiatric patients. Epigenetic changes can lead to improper activation or silencing of genes and have been implicated in a range of diseases. One type of epigenetic change occurs when histones are chemically modified with markers that influence the DNA and proteins that comprise the nucleus of a cell. Two specific histone modifications have been shown to regulate gene transcriptions in the brain. Researchers investigated the role of histone modification in schizophrenia by collecting olfactory neurons via nasal biopsy from four individuals with schizophrenia and comparing them to those of four matched controls. Researchers then analyzed the cells to determine specific genes and gene groups that are affected in expression by epigenetic changes. They identified 22 genes whose expression is likely to be epigenetically modified in schizophrenia.
[No abstract] (Kano S, Colantuoni C, Han F, Zhou Z, Yuan Q, Wilson A, Takayanagi Y, Lee Y, Rapoport J, Eaton W, Cascella N, Ji H, Goldman D, Sawa A. Molecular Psychiatry. 2012 Aug 28 [Epub ahead of print])
Longitudinal Study of the Long-Term Consequences of Drinking During Pregnancy: Heavy in Utero Alcohol Exposure Disrupts the Normal Processes of Brain Development
This longitudinal MRI study showed normal changes in size over time for various regions in the cortical brain in typically developing children but relatively little change in the corresponding regions in children who had been exposed to alcohol prenatally. The severity of these effects was linked to the degree of alcohol exposure, facial dysmorphology (structural changes in the face), and cognitive deficits. Children were 10 to 15 years of age at the time of the study. These results suggest that alcohol-exposed brains are less able to undergo normal developmental changes associated with plasticity and that the trajectory of brain development is affected long after alcohol exposure in utero.
Exposure to alcohol in utero can cause birth defects, including face and brain abnormalities, and is the most common preventable cause of intellectual disabilities. Here we use structural magnetic resonance imaging to measure cortical volume change longitudinally in a cohort of human children and youth with prenatal alcohol exposure (PAE) and a group of unexposed control subjects, demonstrating that the normal processes of brain maturation are disrupted in individuals whose mothers drank heavily during pregnancy. Trajectories of cortical volume change within children and youth with PAE differed from those of unexposed control subjects in posterior brain regions, particularly in the parietal cortex. In these areas, control children appear to show a particularly plastic cortex with a prolonged pattern of cortical volume increases followed by equally vigorous volume loss during adolescence, while the alcohol-exposed participants showed primarily volume loss, demonstrating decreased plasticity. Furthermore, smaller volume changes between scans were associated with lower intelligence and worse facial morphology in both groups, and were related to the amount of PAE during each trimester of pregnancy in the exposed group. This demonstrates that measures of IQ and facial dysmorphology predict, to some degree, the structural brain development that occurs in subsequent years. These results are encouraging in that interventions aimed at altering “experience” over time may improve brain trajectories in individuals with heavy PAE and possibly other neurodevelopmental disorders. (Lebel C, Mattson SN, Riley EP, Jones KL, Adnams CM, May PA, Bookheimer SY, O’Connor MJ, Narr KL, Kan E, Abaryan Z, Sowell ER. Journal of Neuroscience. 2012 Oct 31;32(44):15243-51)
Longitudinal Associations Between Smoking Cessation Medications and Alcohol consumption Among Smokers in the International Tobacco Control Four Country Survey
While quitting smoking does not appear to affect drinking behavior, new researcher suggests that some smoking cessation medications may help to reduce alcohol consumption. After analyzing data from a longitudinal study of nearly 5,000 smokers, researchers found that individuals using varenicline (marketed under the brand name Chantix) reduced their drinking and were less likely to consume alcohol at least once a month than those on nicotine replacement or no medication. People using nicotine replacement were found to be more likely to drink once a month or more compared to those not taking medication. The effects of these medications occurred independent of whether the individual stopped smoking.
Available evidence suggests that quitting smoking does not alter alcohol consumption. However, smoking cessation medications may have a direct impact on alcohol consumption independent of any effects on smoking cessation. Using an international longitudinal epidemiological sample of smokers, we evaluated whether smoking cessation medications altered alcohol consumption independent of quitting smoking. Longitudinal data were analyzed from the International Tobacco Control Four Country (ITC-4) Survey between 2007 and 2008, a telephone survey of nationally representative samples of smokers from the United Kingdom, Australia, Canada, and the United States (n = 4,995). Quantity and frequency of alcohol consumption, use of smoking cessation medications (varenicline, nicotine replacement [NRT], and no medications), and smoking behavior were assessed across 2 yearly waves. Controlling for baseline drinking and changes in smoking status, we evaluated whether smoking cessation medications were associated with reduced alcohol consumption. Varenicline was associated with a reduced likelihood of any drinking compared with nicotine replacement (OR = 0.56; 95% CI = 0.34 to 0.94), and consuming alcohol once a month or more compared to nicotine replacement (OR = 0.43; 95% CI = 0.27 to 0.69) or no medication (OR = 0.63; 95% CI = 0.41 to 0.99). Nicotine replacement was associated with an increased likelihood of consuming alcohol once a month or more compared to no medication (OR = 1.14; 95% CI = 1.03 to 1.25). Smoking cessation medications were not associated with more frequent drinking (once a week or more) or typical quantity consumed per episode. Medication effects on drinking frequency were independent of smoking cessation. This epidemiological investigation demonstrated that varenicline was associated with a reduced frequency of alcohol consumption. Continued work should clarify under what conditions nicotine replacement therapies may increase or decrease patterns of alcohol consumption. (McKee SS, Kelly C, Young-Wolff E, Harrison K, Cummings M, Borland R, Kahler K, Fong G, Hyland A. Alcoholism: Clinical & Experimental Research. 2012 Dec 14 [Epub ahead of print])
Use of treatment strategies in a moderated drinking program for women
This study gives insight into how frequently individuals participating in drinking reduction interventions use the drinking reduction strategies presented during treatment. In this study of 144 women in a 10-week drinking reduction program, those women who drank more prior to entering treatment used fewer drinking reduction strategies during treatment. In addition, those women that used more drinking strategies had reduced drinking, but only in the early post-treatment period.
Little is known about the extent to which individuals participating in drinking reduction interventions use the drinking reduction strategies presented during treatment. In consideration of this issue, we advanced hypotheses about the impact of baseline drinking patterns on strategy use and the relationship of strategy use to drinking patterns over time. One hundred forty-four women who participated in a 10-week drinking reduction program were monitored over an 18-month posttreatment follow-up period. Results indicated that the frequency of baseline heavy drinking days and the frequency of baseline abstinent/light drinking days negatively predicted drinking reduction strategy use during treatment. Over the follow-up period, strategy use decreased; however, participants who received booster sessions had higher strategy use during the initial phase of follow-up. Although cross-lagged panel analysis revealed that strategy use during treatment predicted abstinent/light days at the 6-month follow-up assessment, this effect was moderated by baseline drinking patterns. These data indicated that the use of drinking reduction strategies is predictive of subsequent reduced drinking only in the early posttreatment period and only for baseline heavier drinkers. Future research is needed to further specify the interplay of strategy use and drinking outcomes and to develop interventions designed to encourage the continued use of strategies over extended periods of time. (Mendoza NS, Walitzer KS, Connors GJ. Addictive Behaviors. 2012 Sep;37(9):1054-7)
Striatal dopamine release and genetic variation of the serotonin 2C receptor in humans
NIAAA-supported researchers found that a common variant in a key serotonin receptor gene was linked to greater dopamine release in the striatum, an interior region of the forebrain. Striatal dopamine release plays a crucial role in the rewarding effects of drug use. This is the first study to link this particular variant, Ser23, with dopaminergic response in humans. Using imaging genetics, NIAAA researchers showed that people carrying Ser23 showed greater dopamine release in the nucleus accumbens, caudate nucleus, and putamen after being subjected to pain. The findings have implications for studying mood disorders, addictions, and other stress-related illnesses, which are associated with greater stress-induced dopamine release in these brain regions.
Mesoaccumbal and nigrostriatal projections are sensitive to stress, and heightened stress sensitivity is thought to confer risk for neuropsychiatric disorders. Serotonin 2C (5-HT(2C)) receptors mediate the inhibitory effects of serotonin on dopaminergic circuitry in experimental animals, and preclinical findings have implicated 5-HT(2C) receptors in motivated behaviors and psychotropic drug mechanisms. In humans, a common missense single-nucleotide change (rs6318, Cys23Ser) in the 5-HT(2C) receptor gene (HTR2C) has been associated with altered activity in vitro and with clinical mood disorders. We hypothesized that dopaminergic circuitry would be more sensitive to stress in humans carrying the Ser23 variant. To test this hypothesis, we studied 54 healthy humans using positron emission tomography and the displaceable D(2)/D(3) receptor radiotracer [(11)C]raclopride. Binding potential (BP(ND)) was quantified before and after a standardized stress challenge consisting of 20 min of moderate deep muscular pain, and reduction in BP(ND) served as an index of dopamine release. The Cys23Ser variant was genotyped on a custom array, and ancestry informative markers were used to control for population stratification. We found greater dopamine release in the nucleus accumbens, caudate nucleus, and putamen among Ser23 carriers, after controlling for sex, age, and ancestry. Genotype accounted for 12% of the variance in dopamine release in the nucleus accumbens. There was no association of Cys23Ser with baseline BP(ND). These findings indicate that a putatively functional HTR2C variant (Ser23) is associated with greater striatal dopamine release during pain in healthy humans. Mesoaccumbal stress sensitivity may mediate the effects of HTR2C variation on risk of neuropsychiatric disorders. (Mickey BJ, Sanford BJ, Love TM, Shen PH, Hodgkinson CA, Stohler CS, Goldman D, Zubieta JK. Journal of Neuroscience. 2012 Jul 4;32(27):9344-50)
Impaired Insulin/IGF Signaling in Experimental Alcohol-Related Myopathy
This study provides evidence for a model of alcoholic myopathy, muscle weakness caused by a breakdown in muscle tissue ― one of the less-studied conditions resulting from chronic alcohol abuse. Acute myopathy, which develops during a binge drinking episode or soon after, occurs in about 5 percent of chronic heavy drinkers. Chronic myopathy, characterized by progressive weakness in proximal muscles, occurs in an estimated 33% to 67% of alcoholics. The researchers propose a mechanism for alcoholic myopathy that involves impaired insulin/ insulin-like growth factor (IGF) signaling and generation of lipid peroxides, which can trigger cell death. This paper is one in a continuing theme providing data supporting a unified mechanism for alcohol-induced pathology in a variety of organ systems. The findings suggest that alcohol-related myopathy involves similar mechanisms to those underlying alcoholic steatohepatitis and neurodegeneration.
Alcohol-related myopathy (Alc-M) is highly prevalent among heavy drinkers, although its pathogenesis is not well understood. We hypothesize that Alc-M is mediated by combined effects of insulin/IGF resistance and oxidative stress, similar to the effects of ethanol on liver and brain. We tested this hypothesis using an established model in which adult rats were pair-fed for 8 weeks with isocaloric diets containing 0% (N = 8) or 35.5% (N = 13) ethanol by caloric content. Gastrocnemius muscles were examined by histology, morphometrics, qRT-PCR analysis, and ELISAs. Chronic ethanol feeding reduced myofiber size and mRNA expression of IGF-1 polypeptide, insulin, IGF-1, and IGF-2 receptors, IRS-1, and IRS-2. Multiplex ELISAs demonstrated ethanol-associated inhibition of insulin, IRS-1, Akt, and p70S6K signaling, and increased activation of GSK-3β. In addition, ethanol-exposed muscles had increased 4-hydroxy-2-nonenal immunoreactivity, reflecting lipid peroxidation, and reduced levels of mitochondrial Complex IV, Complex V, and acetylcholinesterase. These results demonstrate that experimental Alc-M is associated with inhibition of insulin/IGF/IRS and downstream signaling that mediates metabolism and cell survival, similar to findings in alcoholic liver and brain degeneration.
Moreover, the increased oxidative stress, which could be mediated by mitochondrial dysfunction, may have led to inhibition of acetylcholinesterase, which itself is sufficient to cause myofiber atrophy and degeneration. (Nguyen VA, Le T, Tong M, Silbermann E, Gundogan F, de la Monte SM. Nutrients. 2012 Aug;4(8):1058-75)
Chronic ethanol increases systemic TLR3 agonist-induced neuroinflammation and neurodegeneration
NIAAA-supported researchers report that chronic alcohol exposure increases risk for inflammation and degeneration of nervous system tissue following an immune response. Previous studies have shown that the immune system produces a cascade of inflammatory molecules that can cross into the central nervous system, causing inflammation and, potentially, degeneration of nerve cells. In this study, mice exposed to alcohol for ten days showed some evidence of nervous system inflammation. However, the combination of chronic alcohol exposure and immune system challenge produced marked evidence of nervous system inflammation and early indications of neurodegeneration, the first such evidence that chronic alcohol and immune challenge increase risk for inflammation of, and damage to, nervous system tissue.
An immunological challenge produces a systemic reaction with the production of cytokines such as TNFalpha that induce systemic inflammation and cross into the CNS and initiate neuroinflammation and potentially neurodegeneration. While the blood levels of cytokines recover a day after an immune challenge, the neuroimmune response in the CNS persists for three days. This study examined the course of the systemic and CNS response to a systemic immune challenge and compared the response following a chronic alcohol exposure. Exposure of mice to ten days of alcohol resulted in some neuroinflammatory response. However the combination of chronic alcohol plus a systemic immune challenge induced a marked neuroinflammatory response and initial indicators of neurodegeneration. These findings provide the first evidence of the significantly increased neuroimune response following chronic alcohol exposure and demonstrate the increased risk of neuroinflammation and neurodegeneration resulting from chronic alcohol exposure. (Qin L, Crews FT. Journal of Neuroinflammation. 2012 Jun 18;9:130-147)
Youth alcohol use and dating abuse victimization and perpetration: a test of the relationships at the daily level in a sample of pediatric emergency department patients who use alcohol
Alcohol use is a potential risk factor for dating abuse among teens and young adults who drink, based on findings from a recent NIAAA study. Researchers gathered responses from patients ages 17 to 21 receiving care in the emergency department and found that drinking was linked to dating abuse victimization and perpetration among both men and women. Both genders were more than twice as likely to commit dating abuse on a heavy drinking day and 1.7 times as likely on a day when they reported any drinking. The risk of victimization increased 23 percent for men and 34 percent for women on days when they had been drinking. These numbers rose to 41 and 43 percent, respectively, when drinking heavily. The authors caution that they did not attempt to establish the order of drinking and abuse during the day, leaving the possibility that some may have consumed alcohol subsequent to the incident.
This study retrospectively examined the daily-level associations between youth alcohol use and dating abuse (DA) victimization and perpetration for a 6-month period. Timeline Followback (TLFB) interview data were collected from 397 urban emergency department patients, ages 17 to 21 years. Patients were eligible if they reported past month alcohol use and past year dating. Generalized estimating equation (GEE) analyses estimated the likelihood of DA on a given day as a function of alcohol use or heavy use (≥4 drinks per day for women, ≥5 drinks per day for men), as compared with nonuse. Approximately 52% of men and 61% of women participants reported experiencing DA victimization ≥1 times during the past 6 months, and 45% of men and 55% of women reported perpetrating DA ≥1 times. For both men and women, DA perpetration was more likely on a drinking day as opposed to a nondrinking day (ORs = 1.70 and ORs = 1.69, respectively). DA victimization was also more likely on a drinking day as opposed to a nondrinking day for both men and women (ORs = 1.23 and ORs = 1.34, respectively). DA perpetration and DA victimization were both more likely on heavy drinking days as opposed to nondrinking days (2.04 and 2.03 for men's and women's perpetration, respectively, and 1.41 and 1.43 for men's and women's victimization, respectively). This study found that alcohol use was associated with increased risk for same day DA perpetration and victimization, for both male and female youth. We conclude that for youth who use alcohol, alcohol use is a potential risk factor for DA victimization and perpetration. (Rothman EF, Stuart GL, Winter M, Wang N, Bowen DJ, Bernstein J, Vinci R. Journal of Interpersonal Violence. 2012 Oct;27(15):2959-79)
S-adenosyl methionine regulates ubiquitin-conjugating enzyme 9 protein expression and sumoylation in murine liver and human cancers
Ubiquitin is a small protein involved in a host of cell processes including DNA repair, the regulation of transcription, and apoptosis (programmed cell death). The process of marking a protein with ubiquitin, called ubiquitination, is emerging as a key regulatory mechanism in both normal and cancerous cells. NIAAA researchers have found that a key enzyme involved in the ubiquitination process, Ubc9, is
hyperphosphorylated in multiple cancers. Hyperphosphorylation plays a role in regulating cell mitosis. In the current study, researchers found that the hyperphosporylation of Ubc9 can be normalized with SAMe, a naturally occurring compound produced from methionine, and its metabolite, MTA. This finding has important implications for carcinogenesis and possible cancer chemotherapy.
Ubiquitin-conjugating enzyme 9 (Ubc9) is required for sumoylation and is overexpressed in several malignancies, but its expression in hepatocellular carcinoma (HCC) is unknown. Hepatic S-adenosyl methionine (SAMe) levels decrease in methionine adenosyltransferase 1A (Mat1a) knockout (KO) mice, which develop HCC, and in ethanol-fed mice. We examined the regulation of Ubc9 by SAMe in murine liver and human HCC, breast, and colon carcinoma cell lines and specimens. Real-time polymerase chain reaction and western blotting measured gene and protein expression, respectively. Immunoprecipitation followed by western blotting examined protein-protein interactions. Ubc9 expression increased in HCC and when hepatic SAMe levels decreased. SAMe treatment in Mat1a KO mice reduced Ubc9 protein, but not messenger RNA (mRNA) levels, and lowered sumoylation. Similarly, treatment of liver cancer cell lines HepG2 and Huh7, colon cancer cell line RKO, and breast cancer cell line MCF-7 with SAMe or its metabolite 5'-methylthioadenosine (MTA) reduced only Ubc9 protein level. Ubc9 posttranslational regulation is unknown. Ubc9 sequence predicted a possible phosphorylation site by cell division cycle 2 (Cdc2), which directly phosphorylated recombinant Ubc9. Mat1a KO mice had higher phosphorylated (phospho)-Ubc9 levels, which normalized after SAMe treatment. SAMe and MTA treatment lowered Cdc2 mRNA and protein levels, as well as phospho-Ubc9 and protein sumoylation in liver, colon, and breast cancer cells. Serine 71 of Ubc9 was required for phosphorylation, interaction with Cdc2, and protein stability. Cdc2, Ubc9, and phospho-Ubc9 levels increased in human liver, breast, and colon cancers. Cdc2 expression is increased and Ubc9 is hyperphosphorylated in several cancers, and this represents a novel mechanism to maintain high Ubc9 protein expression that can be inhibited by SAMe and MTA. (Tomasi ML, Tomasi I, Ramani K, Pascale RM, Xu J, Giordano P, Mato JM, Lu SC. Hepatology. 2012 Sep;56(3):982-93)
Ethanol-Induced Mast Cell-Mediated Inflammation Leads to Increased Susceptibility of Intestinal Tumorigenesis in the APC (Δ468) Min Mouse Model of Colon Cancer
Chronic and frequent alcohol use has been associated with an increased incidence of several types of cancers. Although the underlying mechanism of alcohol’s cancer-causing effect has not been clearly established, inflammation may be a common feature of alcohol-related cancers. NIAAA-supported researchers recently showed that intestinal mast cells, which play a key role in the inflammatory process, play a central role in intestinal carcinogenesis. In this study, they examined whether mast cell-mediated inflammation is a mechanism by which chronic alcohol promotes intestinal cancer. Using mice that are genetically susceptible to intestinal polyps, they found that alcohol increased both polyp number and size within the small and the large intestines, that only alcohol-fed mice showed evidence of tumor invasion, and that chronic alcohol feeding increased mast cell number and activity. The findings suggest that mast cell-mediated inflammation could be a mechanism by which alcohol promotes carcinogenesis.
Chronic and frequent alcohol (ethanol) intake has been associated with an increased incidence of several types of cancers including breast, mouth, throat, esophageal, stomach, and colorectal. The underlying mechanism of this deleterious carcinogenic effect of alcohol has not been clearly established but inflammation may be 1 unifying feature of these cancers. We have recently shown that intestinal mast cells play a central role in intestinal carcinogenesis. In this study, we tested our hypothesis that mast cell-mediated inflammation is 1 underlying mechanism by which chronic alcohol promotes intestinal tumorigenesis. APCD468 mice were fed either an alcohol-containing Nanji liquid diet or isocaloric dextrose-containing Nanji diet for 10 weeks and then sacrificed to collect small and large intestine samples. Assessments of tumor number and size as well as mast cell number and mast cell activity and histology score for invasion were compared between Control (dextrose-fed) and alcohol-fed APCD468 mice. The effect of alcohol on mast cell-mediated tumor migration was also assessed using an in vitro migration assay. Results: Alcohol feeding increased both polyp number and size within both the small and the large intestines of APCD468 mice. Only alcohol-fed mice showed evidence of tumor invasion. Chronic alcohol feeding also resulted in an increased mast cell number and activity in tumor stroma and invading borders. In vitro migration assay showed that alcohol significantly increases mast cell-mediated tumor migration in vitro. Our data show that chronic alcohol intake promotes: (i) intestinal tumorigenesis and tumor invasion in genetically susceptible mice; (ii) increases in polyp-associated mast cells; and (iii) mast cell-mediated tumor migration in vitro. Both our in vivo and in vitro studies suggest that mast cell-mediated inflammation could be 1 mechanism by which alcohol promotes carcinogenesis. (Wimberly, AL, Forsyth, CB, Khan, MW, Pemberton, A, Khazaie, K and Keshavarzian, A. Alcoholism: Clinical & Experimental Research. 2013 Jan;37 Suppl 1:E199-208)

