NIAAA Director's Report on Institute Activities to the 139th Meeting of the National Advisory Council on Alcohol Abuse and Alcoholism
Table of Contents
- NIAAA BUDGET
- LEGISLATIVE NEWS
- COLLABORATIVE RESEARCH ON ADDICTION AT NIH UPDATE
- DIRECTOR'S ACTIVITIES
- STAFF TRANSITIONS
- HONORS AND AWARDS
- NEW NOTICE OF FUNDING OPPORTUNITIES
- NOTABLE NIAAA STAFF ACTIVITIES
- WHAT'S AHEAD
- NIH RESEARCH HIGHLIGHTS
- NIAAA COMMUNICATIONS, OUTREACH & MEDIA COVERAGE
FY 2015
After a lengthy continuing resolution, HR 83, the Consolidated and Further Continuing Appropriations Act for fiscal year (FY) 2015, was signed by President Obama on December 16, 2014. The National Institutes of Health (NIH) received a total of $30.3 billion, $150 million above FY 2014 level. The bill includes specific increases for Alzheimer’s disease, cancer, and the BRAIN initiative, as well as $12.6 million for the Gabriella Miller Kids First Research Act to support pediatric research.
The FY 2015 appropriation for NIAAA provides $447.2 million. This represents a $0.9 million or a 0.3 percent increase over the FY 2014 budget level. NIAAA estimates it will support a total of 697 research project grants (RPGs) in FY 2015, including 167 competing awards.
FY 2016
On February 2, 2015, President Obama submitted to Congress his FY 2016 budget request for all Federal agencies – the FY 2016 President’s Budget. Included in this request is a proposed FY 2016 budget for the NIH of $31.3 billion. The NIAAA budget request for FY 2016 is $459.8 million, a $12.7 million or 2.8 percent increase over the FY 2015 enacted level.
NIAAA Budget Mechanism - Total
(Dollars in Thousands)
|
MECHANISM |
FY 2015 ENACTED |
FY 2016 PRESIDENT'S BUDGET |
||
|---|---|---|---|---|
|
|
No. |
Amount |
No. |
Amount |
|
Research Projects |
|
|
|
|
|
Noncompeting |
501 |
$189,337 |
491 |
$186,684 |
|
Administrative Supplements * |
(24) |
1,269 |
(24) |
1,269 |
|
Competing |
167 |
51,874 |
176 |
59,120 |
|
Subtotal, RPGs |
668 |
242,480 |
667 |
247,073 |
|
SBIR/STTR |
29 |
10,955 |
37 |
11,889 |
|
Research Project Grants |
697 |
253,435 |
704 |
258,962 |
|
Research Centers |
|
|
|
|
|
Specialized/Comprehensive |
18 |
28,446 |
17 |
28,200 |
|
Clinical Research |
- |
- |
- |
- |
|
Biotechnology |
- |
- |
- |
- |
|
Comparative Medicine |
- |
- |
- |
- |
|
Res. Centers in Minority Instit. |
- |
- |
- |
- |
|
Subtotal, Centers |
18 |
28,446 |
17 |
28,200 |
|
Other Research |
|
|
|
|
|
Research Careers |
93 |
13,834 |
93 |
14,000 |
|
Cancer Education |
- |
- |
- |
|
|
Cooperative Clinical Research |
1 |
7,180 |
1 |
7,180 |
|
Biomedical Research Support |
- |
- |
- |
|
|
Minority Biomed. Res. Support |
- |
340 |
- |
|
|
Other |
42 |
14,254 |
46 |
15,000 |
|
Subtotal, Other Research |
136 |
35,608 |
140 |
36,180 |
|
Total Research Grants |
851 |
317,489 |
861 |
323,342 |
|
|
|
|
|
|
|
Training |
|
|
|
|
|
Individual |
95 |
4,274 |
99 |
4,500 |
|
Institutional |
174 |
8,415 |
175 |
8,700 |
|
Total Training |
269 |
12,689 |
274 |
13,200 |
|
Research & Develop. Contracts |
68 |
37,035 |
69 |
42,552 |
|
(SBIR/STTR) * |
(4) |
(1,091) |
(4) |
(1,100) |
|
|
|
|
|
|
|
Intramural Research |
108 |
49,496 |
109 |
49,991 |
|
Res. Management & Support |
128 |
30,444 |
128 |
30,748 |
|
|
|
|
|
|
|
Total, NIAAA Budget Authority |
|
$447,153 |
|
$459,833 |
Precision Medicine Initiative
President Obama launched his Precision Medicine Initiative in January 2015 with the goal of accelerating biomedical discoveries and providing clinicians with new tools, knowledge, and therapies to select which treatments work best for which patients. NIH will play a large role in this initiative by: 1) creating a national research cohort of one million voluntary participants to propel our understanding of health and disease; and 2) expanding efforts to identify genomic drivers in cancer and to apply that knowledge in the development of more effective approaches to cancer treatment. The FY 2016 initiative would provide a $215 million investment to NIH, the Food and Drug Administration (FDA), and the Office of the National Coordinator for Health Information Technology.
21st Century Cures Initiative
Led by Rep. Fred Upton, Chairman of the House Energy and Commerce Committee, the goal of this initiative is to enhance and accelerate the discovery, development, and delivery of new treatments and cures. While most of the provisions of the proposed bill apply to FDA, some provisions are applicable to NIH. For example, the bill would establish an NIH innovation fund, to be provided $2 billion in mandatory funds each year from FY 2016 through FY 2020 and increase loan repayment limits for young emerging scientists. The bill passed unanimously out of the House Energy and Commerce Committee on May 21, 2015 and is due to be debated by the full House.
COLLABORATIVE RESEARCH ON ADDICTION AT NIH UPDATE
The Adolescent Brain Cognitive Development (ABCD) Study is a national longitudinal study that will assess the short- and long-term impact of substance use on brain development. The project will recruit 10,000 youths before they begin using alcohol, marijuana, tobacco, and other drugs, and will follow them over ten years into early adulthood. April 14, 2015 was the closing date for applications responding to the three ABCD Study Notice of Funding Opportunities (NOFOs) which received an excellent level of response. Peer review of these applications is scheduled for mid-July, and awards are anticipated by September 30, 2015.
On May 12-13, 2015, NIH convened a meeting for recipients of CRAN research supplements. Forty grantees and several NIH scientific staff attended, representing a wide range of research from basic science to clinical and health services research, including quality of life studies. Through one and a half days of research presentations, poster sessions, panel discussions, and informal interaction, participants identified the challenges and opportunities of conducting multi-substance research. NIAAA Director, Dr. George Koob, led with a plenary talk that presented his conceptual framework of addiction. He also highlighted research advances in the neurobiology of addiction relevant to this framework with a focus on the “dark side” of addiction and common neuroplasticity across drugs of abuse and alcohol. The mix of both new and senior investigators as well as transdisciplinary topic areas resulted in a rich discussion. The meeting summary that will be available by September, 2015.
DIRECTOR’S ACTIVITIES - DECEMBER 2014-MAY 2015
Dr. Koob gave an “Update on Research on Alcohol Use Disorders at NIAAA” presentation on December 7, 2014 at the American College of Neuropsychopharmacology (ACNP) meeting.
On January 27, 2015, Dr. Koob was a speaker at the University of California San Diego Psychiatry Department Grand Rounds. The title of his talk was “Neurobiology of Addiction: A View from the Dark Side.”
Dr. Koob spoke at the Community Anti-Drug Coalitions of America (CADCA) National Leadership Forum on February 3, 2015. His topic was “NIAAA: Current Priorities and Future Goals.”
On March 12, 2015, Dr. Koob presented a seminar, “How Does Science Inform Diagnosis, Prevention and Treatment of Alcoholism?” at the University of Puerto Rico.
Dr. Koob gave the Common Hour Talk on March 26, 2015 at Franklin & Marshall College. The title was “Drugs, Pleasure and Pain: The Two Faces of Janus.”
On April 1, 2015, Dr. Koob gave the Sprague Lecture at the 31st Retreat/Symposia of the Mahoney Institute of the University of Pennsylvania. The lecture was on the “Neurobiological Bases for Opponent Processes in Drug Addiction.”
Dr. Koob was a lecturer at the April 10, 2015 Anxiety and Depression Association of America meeting in Miami, FL. His topic was “The Intersection of Depression, Anxiety, and Addiction.”
Dr. Koob was the R. Brinkley Smithers Award speaker on April 24, 2015 at the 46th Annual American Society of Addiction Medicine meeting. The title of his talk was “Reward, Stress and Addiction: Two Faces of Janus.”
Dr. Koob was the Plenary Lecture Speaker at the 2015 Society of Biological Psychiatry meeting on May 15, 2015 in Toronto, Canada. The topic of his speech was “Addiction as a Stress Surfeit Disorder.”
On May 19, 2015, Dr. Koob spoke at the American Psychiatric Association’s 68th annual meeting. His topic was “How Science Can Inform the Diagnosis, Prevention and Treatment of Alcohol Use Disorders.”
Dr. Koob gave a lecture on May 27, 2015 at the Uniformed Services University in Bethesda, MD, titled “Reward and Stress in the Neurobiology of Addiction: The Two Faces of Janus.
Cara Breeden joined the Communications and Public Liaison Branch on May 31, 2015 as a technical writer-editor and will serve as our publications manager along with her other duties. She comes to NIAAA from National Institute of Allergy and Infectious Diseases (NIAID), where she managed a range of writing, editing, outreach, and special events activities. Prior to her time at NIAID, Cara served as a Technical Information Specialist at the National Library of Medicine and as a Senior Health Information Specialist at the American Institutes for Research in Frederick, MD. She also taught English at the International Center for Pedagogical Studies in Hautes-de-Seine, France. Cara is a Phi Beta Kappa graduate of Davidson College with a degree in French and Medical Humanities, and has a Masters of Library Science degree from Texas Woman’s University with a concentration in health sciences. Cara has received numerous performance awards and commendations from multiple organizations.

Vicki Buckley joined the Office of Resource Management in May 2015, as the Deputy Executive Officer for NIAAA. Prior to joining NIAAA, Vicki served as the Deputy Executive Officer/Acting Executive Officer for the National Eye Institute (NEI) since January, 2013. Prior to NEI, she worked at the National Institute on Mental Health (NIMH) from 1999 to 2013, serving in numerous administrative roles including over three years as the Chief Administrative Officer for the NIMH Intramural Research Program. Vicki has an extensive background in NIH administration including financial management, acquisitions, property management, human resources, and policy and management analysis. Vicki earned a B.S. in Health Care Management from Southern Illinois University, and a Master’s in Business Administration from Mt. Saint Mary’s University.

Karen Harrington joined the Office of Resource Management in March 2015, as the Chief of the Intramural Administrative Management Section. Before joining NIAAA, Karen worked for the National Cancer Institute since 2009 as a Lead Administrative Officer with the Center for Cancer Research, Basic Research Administrative Resource Center (ARC). In this role, Karen led a team of Administrative Officers providing a full complement of administrative services, and she served as the travel expert for the ARC. Prior to this role, Karen was a servicing Administrative Officer for the Laboratory of Cell Biology, headed by Dr. Michael Gottesman.

Jon’lethia King joined the NIAAA Office of the Director as a Staff Assistant on April 20, 2015. Jon'lethia has almost six years of experience at the NIH, including four years with the National Institute of Neurological Disorders and Stroke (NINDS) as an Extramural Support Assistant and most recently as a Human Resources Assistant with the Office of Human Resources. She supported the Program Director at NINDS, providing analysis for new research studies and tracking the milestone requirements necessary for continued grant funding. Jon'lethia also provided program support on ground breaking initiatives leading to an NIH Director's Award. Jon'lethia has a Bachelor of Science in Sociology and a Graduate Certificate in Human Resources. She is currently considering Drexel University for a Master's Degree

Dr. Mariela Shirly returned to NIAAA as a Health Scientist Administrator in the Division of Epidemiology and Prevention Research (DEPR). For the past two years, Mariela served in the Office of Research on Women’s Health in the Office of the Director, NIH. Dr. Shirley earned a Ph.D. in clinical psychology from Vanderbilt University. She is a fellow of the American Psychological Association and in 2012 received the APA Meritorious Research Service Commendation Award. Her research expertise areas include behavioral interventions, psychiatric comorbidity, and behavioral medicine. Her DEPR research portfolio focuses on screening and brief interventions, underage/college drinking, military/veterans, and psychiatric and other drug comorbidity.

Jeff Thurston joined the NIAAA Grants Management Branch as a Grants Management Specialist on May 4, 2015. Jeff, a former NIH Grants Management Specialist at the National Institute of Arthritis, Musculoskeletal and Skin Diseases and the National Institute of Dental and Craniofacial Research, has returned to NIH from his most recent position as the Research Operations Coordinator in the Center for Childhood Cancer and Blood Diseases at the Research Institute at Nationwide Children’s Hospital (NCH) in Ohio. At NCH Jeff was responsible for creating and organizing the Center’s grant program. He also conducted training for NCH faculty and fellows, as well as the NIH grants management community and the Society of Research Administrators International at its annual meeting. He received his Bachelor of Arts in Political Science from the University of Colorado at Denver.

Dr. Aaron White joined the Office of the Director, as Senior Advisor to the Director for Research and Statistics. Trained as a neuroscientist, Dr. White will be involved in strategic planning for the Institute as well as providing valuable statistical expertise. From 2008-2015, Dr. White was a program official in NIAAA’s Division of Epidemiology and Prevention Research, where he maintained a portfolio of grants on underage and college drinking epidemiology and prevention studies. Prior to joining NIH, he was an assistant professor at Duke University Medical Center.

Kelvin Zeigler joined the NIAAA Grants Management Branch as a Grants Management Specialist, effective March 9, 2015. Kelvin joins NIAAA from the National Institute for Neurological Disorders and Stroke (NINDS), where he served as a Grants Management Specialist since 2010. Prior to joining NINDS, he worked at the National Cancer Institute holding several positions beginning in 2006 through 2010. Kelvin completed the NIH Administrative Fellows Program in 2012. In addition, Kelvin served in the U.S. Navy from 1998-2006, where he received numerous commendations. Kelvin received his Bachelor’s degree in Health Care Management at Southern Illinois University at Carbondale.
Jo-Ann Kriebel, who served as a Writer/Editor in the NIAAA Communications and Public Liaison Branch, has taken a position as a technical writer-editor at the National Institute of Nursing Research.
James Padgett, who served as an Extramural Support Assistant in the Grants Management Branch, has left NIAAA for a position as a Grants Management Specialist with the Substance Abuse and Mental Health Services Administration.
Dr. Adeline Bertola received the 2015 NIAAA Daniel Hommer award for characterizing a new mouse model of alcoholic liver injury induced by chronic-plus-binge ethanol feeding, which was published in Nature Protocols in 2013. This new mouse model has now been used by many laboratories around the world.
Dr. Dechun Feng received the 2015 NIH Fellows Award for Research Excellence for establishing a new mouse model of cell ablation by generating a Cre-inducible CD59 transgenic mice. This model can be used to specifically delete different types of cells in mice and study their functions in vivo.
Dr. David Goldman is the recipient of the 36th Annual Research Society on Alcoholism (RSA) Distinguished Researcher Award. This award is given to an individual who has made significant contributions to the study of alcohol abuse and alcoholism and who has demonstrated leadership in the field. Dr. Goldman will present a plenary lecture titled “Genetic Pathways to Alcoholism” at the 2015 RSA meeting in San Antonio, TX.
Dr. George Koob received the R. Brinkley Smithers Distinguished Scientist Award from the American Society of Addiction Medicine. This award recognizes and honors an individual who has made highly meritorious contributions in advancing the scientific understanding of alcoholism, its prevention, and treatment.
Dr. Man Li was selected for an oral presentation in a plenary session and a travel award at the 2015 Digestive Disease Week meeting in Washington, D.C.
Dr. Raye Litten, Dr. Joanne Fertig, Ms. Megan Ryan, and Dr. Daniel Falk were awarded the NIAAA 2015 Scientific Achievement Group Award for their leadership in medications development through the NIAAA Clinical Investigations Group.
Dr. Marcia Scott was recently selected as a 2015 recipient of the American Psychological Association Meritorious Research Service Commendation for her outstanding contributions to psychological science.
NEW NOTICE OF FUNDING OPPORTUNITIES (NOFOs)
The following Requests for Applications (RFAs) and Program Announcements (PAs) were issued by NIAAA:
RFA-AA-15-001: Specialized Alcohol Research Centers (P50). This RFA solicits applications for specialized Alcohol Research Centers to provide leadership in conducting and fostering interdisciplinary, collaborative research on a wide variety of topics relevant to the Institute’s mission.
PAR-15-153: Investigational New Drug (IND)-enabling Development of Medications to Treat Alcohol Use Disorder and Alcohol-related Disorders (UT2). This NOFO directed to Small Business Technology Transfer applicants is dedicated to the development of therapeutic agents for disorders that fall under the mission of NIAAA. The NOFO supports IND-enabling studies for candidate therapeutic agents.
PAR-15-154: Investigational New Drug (IND)-enabling Development of Medications to Treat Alcohol Use Disorder and Alcohol-related Disorders (U44). This NOFO encourages Small Business Innovation Research (SBIR) applications from small business concerns (SBCs) that propose the development of therapeutic agents for disorders that fall under the mission of NIAAA. The NOFO supports IND-enabling studies for candidate therapeutic agents.
PAR-15-184: Summer Research Education Experience Programs (R25). The NIH Research Education Program (R25) supports research education activities in the mission areas of the NIH. The over-arching goal of this R25 program is to support educational activities that foster a better understanding of biomedical, behavioral, and clinical research and its implications. To accomplish the stated over-arching goal, this NOFO will support creative educational activities with a primary focus on research experiences for high school, undergraduate, and science teachers during the summer academic break.
PA-15-159: Alcohol Impairment of Immune Function, Host Defense and Tissue Homeostasis (R01). This re-released PA invites applications from researchers with broad expertise to study the consequences of alcohol consumption on immune function with a goal toward improving the outcome of patients who abuse alcohol.
PA-15-254: Human Studies to Evaluate Promising Medications to Treat Alcohol Use Disorder (R21). The objective of this NOFO is to encourage investigators who use human laboratory paradigms and/or clinical trials to submit exploratory and developmental proposals to evaluate the safety and efficacy of novel or re-purposed compounds that bind to new targets for treatment of alcohol use disorder (AUD) or AUD with a comorbid post-traumatic stress disorder.
PA-15-255: Human Studies to Evaluate Promising Medications to Treat Alcohol Use Disorder (R03). The objective of this NOFO is to encourage applications that use human laboratory paradigms and/or clinical trials to evaluate the safety and efficacy of novel or re-purposed compounds, that bind to new targets, for treatment of AUD or AUD with a comorbid post-traumatic stress disorder. The R03 small grant supports discrete, well-defined projects that realistically can be completed in two years and that require limited levels of funding.
PA-15-256: Human Studies to Evaluate Promising Medications to Treat Alcohol Use Disorder (R01). The objective of this NOFO is to encourage applications that use human laboratory paradigms and/or clinical trials to evaluate the safety and efficacy of novel or re-purposed compounds, that bind to new targets, for treatment of AUD or AUD with a comorbid post-traumatic stress disorder.
NIAAA is participating in the following NOFOs:
RFA-OD-15-004 (ODP): Tobacco Regulatory Science Small Grant Program for New Investigators (R03). The purpose of this NOFO is to support new investigators in the biomedical, behavioral, and social sciences who are in the early stages of establishing independent careers in tobacco regulatory research.
RFA-EB-15-005 (NIBIB): Neuroimaging Informatics Tools and Resources Clearinghouse (U24). The purpose of this NOFO is to support the Neuroimaging Informatics Tools and Resources Clearinghouse and to enable collaborative research in neuroimaging informatics.
RFA-CA-15-006 (NCI): Big Data to Knowledge (BD2K) Advancing Biomedical Science Using Crowdsourcing and Interactive Digital Media (UH2). The purpose of this Big Data to Knowledge NOFO is to support the development of new or significantly adapted interactive digital media that engages the public, experts or non-experts, in performing some aspect of biomedical research via crowdsourcing.
RFA-AI-15-020 (NIAID): NIH-PEPFAR Collaboration on Implementation Science for HIV: Towards an AIDS-free Generation (R01). The NIH, in collaboration with the Office of the Global AIDS Coordinator (OGAC), is soliciting applications for implementation science research that will inform delivery and scale-up of efficacious interventions to improve HIV prevention, care, and treatment in Africa.
RFA-AI-15-021 (NIAID): NIH-PEPFAR Collaboration on Implementation Science for HIV: Towards an AIDS-free Generation (R21). The NIH, in collaboration with the Office of the Global AIDS Coordinator (OGAC), is soliciting applications for implementation science research that will inform delivery and scale-up of efficacious interventions to improve HIV prevention, care, and treatment in Africa.
RFA-MH-16-160 (NIMH): Lifespan Human Connectome Project: Baby Connectome (U01). This NOFO is issued as an initiative of the NIH Blueprint for Neuroscience Research. The Neuroscience Blueprint is a collaborative framework through which 15 NIH Institutes, Centers, and Offices jointly support neuroscience-related research, with the aim of accelerating discoveries and reducing the burden of nervous system disorders.
PAR-15-121 (NINDS): BRAIN Initiative: Optimization of Novel Tools and Technologies for Neuroscience Research (R44). This NOFO solicits applications through the Small Business Innovation Research program for the optimization of existing and emerging technologies and approaches in neurosciences.
PAR-15-170 (NIDDK): Diet and Physical Activity Assessment Methodology (R01). This NOFO encourages innovative research to enhance the quality of measurements of dietary intake and physical activity.
PAR-15-171 (NIDDK): Diet and Physical Activity Assessment Methodology (R21). This NOFO encourages exploratory and developmental research to enhance the quality of measurements of dietary intake and physical activity.
PAR-15-178 (NINDS): Jointly Sponsored Ruth L. Kirschstein National Research Service Award Institutional Predoctoral Training Program in the Neurosciences (T32). This NOFO supports broad and fundamental research training in the neurosciences via institutional NRSA research training grants (T32) at domestic institutions of higher education. The primary objective is to prepare individuals for careers in neuroscience that have a significant impact on the health-related research needs of the nation.
PA-15-137 (NIA): Administrative Supplements for Research on HIV/AIDS and Aging (Admin Supp). The Office of AIDS Research, in collaboration with the NIH Institutes and Centers named in the NOFO, encourages applications for administrative supplements to fund innovative research on HIV and aging through clinical, translational, observational, or interventional studies in domestic or international settings.
PA-15-177 (NIDA): Pilot and Feasibility Studies in Preparation for Drug and Alcohol Abuse Prevention Trials (R34). This NOFO for R34 applications seeks to support pilot and/or feasibility testing of innovative new, revised, or adapted prevention intervention approaches to prevent or delay the initiation and onset of drug and alcohol use.
PA-15-183 (NIH): Administrative Supplements for Tobacco Regulatory Research on Tobacco Flavors and Flavorings (Admin Supp). The purpose of this NOFO is to generate data related to flavors and flavorings in cigarettes, cigars (including little cigars and cigarillos), and e-cigarettes.
PA-15-188 (NIDA): Developing the Therapeutic Potential of the Endocannabinoid System for Pain Treatment (R01). The purpose of this NOFO is to support projects that will elucidate the therapeutic potential of cannabinoids and the endocannabinoid system in the development of mechanism-based therapies for pain.
PA-15-249 (NLM): Administrative Supplements for Informationist Services in NIH-funded Research Projects (Admin Supp). These administrative supplements provide funds to active awards of participating Institutes and Centers in order to enhance the storage, organization, management and use of electronic research data through the involvement of informationists, also known as in-context information specialists.
PA-15-250 (NIDA): Pilot Health Services and Economic Research on the Treatment of Drug, Alcohol, and Tobacco Abuse (R34). The purpose of this NOFO is to encourage pilot and preliminary research in preparation for larger-scale services research effectiveness trials. Relevant trials may test a wide range of approaches, including interventions, practices, and policies, designed to optimize access to, and the quality, effectiveness, affordability and utilization of drug, tobacco, or alcohol use disorder treatments and related services, as well as services for comorbid medical and mental disorder conditions.
PA-15-251 (NIDA): Health Services and Economic Research on the Prevention and Treatment of Drug, Alcohol, and Tobacco Abuse (R01). This NOFO encourages R01 grant applications to conduct rigorous health services and economic research to maximize the delivery of efficient, high-quality drug, tobacco, and alcohol prevention, treatment, and recovery support services.
PA-15-252 (NIDA): Health Services and Economic Research on the Prevention and Treatment of Drug, Alcohol, and Tobacco Abuse (R03). This NOFO encourages small grant applications to conduct rigorous health services and economic research to maximize the delivery of efficient, high-quality drug, tobacco, and alcohol prevention, treatment, and recovery support services.
PA-15-253 (NIDA): Health Services and Economic Research on the Prevention and Treatment of Drug, Alcohol, and Tobacco Abuse (R21). This NOFO encourages grant applications to conduct rigorous health services and economic research to maximize the delivery of efficient, high-quality drug, tobacco, and alcohol prevention, treatment, and recovery support services.
PA-15-258 (ODS): Administrative Supplements for Research on Dietary Supplements (Admin Supp). This NOFO announces availability ofthe administrative supplements to support research in which the supplemental funding would investigate the role of dietary supplements and/or their ingredients in health maintenance and disease prevention.
NOTABLE NIAAA STAFF ACTIVITIES - FEBRUARY - MAY 2015
Dr. Daniel Falk presented, "Giving and Getting Help for Alcohol Problems: 'Rethinking Drinking' and NIAAA’s New Guide to Treatment Options" at the Community Anti-Drug Coalitions of America (CADCA) 25th Annual National Leadership Forum on February 3, 2015 in National Harbor, MD.
Gregory Bloss co-chaired a workshop on February 25, 2015 to engage a range of stakeholders in discussions about how NIH-funded research can enhance the role of personalized medicine in improving the efficiency and effectiveness of health care. The workshop was convened by the NIH Common Fund Health Economics Program and the steering committee for the Common Fund initiative on Determinants and Consequences of Personalized Health Care and Prevention. Participants included investigators leading cooperative agreements funded under this initiative and invited panelists representing five broad stakeholder groups: (1) health care providers, (2) patient advocates, (3) guidelines organizations, (4) insurers, payers, and health technology assessment organizations, and (5) pharmaceutical and diagnostic developers, manufacturers, and regulators. A report of the workshop is available at: http://commonfund.nih.gov/Healtheconomics/index.
Drs. Ivana Grakalic, Soundar Regunathan, Diana Urbanas, and Ms. Jessica Ryan presented the “Cool Spot Carnival” at the National Museum of Health and Medicine at Walter Reed Army Medical Center as part of the museum’s 16th annual Brain Awareness Week on March 11-12, 2015 organized by the Dana Alliance for Brain Initiatives. This event is an international partnership of government agencies, scientific organizations, university, and volunteer groups dedicated to advancing education about the brain.
Dr. Robert B. Huebner co-chaired a symposium entitled “Searching for the Core of Addiction: Translational Perspectives” at the inaugural meeting of the International Convention of Psychological Science. The conference took place March 12-14, 2015 in Amsterdam, The Netherlands.
Dr. Raye Litten presented “Exploration of Endpoints for Pivotal Clinical Trials to Treat AUD” at the Measures of Outcome for Stimulant Trials conference in Rockville, MD in March, 2015.
Dr. Svetlana Radaeva and Dr. Gary Murray convened a meeting on March 16, 2015 of investigators collaborating in the Alcoholic Hepatitis Consortia to establish common data elements and reporting processes and discuss future clinical studies on alcoholic liver disease.
Dr. Ralph Hingson gave a talk titled “Recent Trends and Findings Regarding the Magnitude and Prevention of College Drinking and Drug Use Problems” at the Substance Abuse and Mental Health Services Administration’s Summit on Behavioral Health Issues among College Students in Rockville, MD, on March 16, 2015. This talk addressed how to best prevent and reduce drinking and drug use and related problems among college students. Dr. Vivian Faden presented on NIAAA’s College Alcohol Interventions Matrix (CollegeAIM) tool designed to help colleges select among evidence-based programs at the same meeting.
Dr. Ralph Hingson gave a talk titled “New Research since the Surgeon General’s Call to Action to Prevent and Reduce Underage Drinking” at Lifesavers: National Conference on Highway Safety Priorities in Chicago, Illinois, on March 17, 2015. This talk outlined new research on trends in and consequences of underage drinking and interventions to prevent and reduce underage drinking that have emerged since the 2007 Surgeon General’s Call to Action to Prevent and Reduce Underage Drinking.
Dr. Raye Litten, Dr. Joanne Fertig, Ms. Megan Ryan, and Dr. Daniel Falk held the Kick-Off meeting for the NIAAA Clinical Investigations Group (NCIG) HORIZANT® (gabapentin enacarbil) study. This meeting was held March 30-31, 2015 in Bethesda, MD.
Dr. Rosalind Breslow gave two presentations titled “Alcohol Use and Association with Dietary Intake” and "Research Gaps and Future Directions” at an Experimental Biology Symposium sponsored by the American Society for Nutrition in Boston, Massachusetts on April 1, 2015. Her presentations focused on issues concerning moderate drinking, nutrition, and chronic diseases.
Dr. Kenneth Warren, was a featured speaker at Congressional briefing sponsored by the Friends of NIAAA on April 13, 2015. The topic of the briefing was “Alcohol and Pregnancy: An Overview of Fetal Alcohol Spectrum Disorders.”
Dr. Bill Dunty presented remarks during the “Funding Opportunities for Cancer Research at NIH” session at the American Association for Cancer Research annual meeting, held on April 21, 2015 in Philadelphia, PA.
Dr. Matthew Reilly attended the Society on Neuroimmune Pharmacology meeting in Miami, Florida on April 22-25, 2015. He participated in the “NeuroAids and Alcohol” satellite event and served as a judge for presentations delivered by young-investigators. In addition, he was part of a speed-mentoring panel that gave advice on grant writing and career development to young investigators.
Dr. Bill Dunty participated in the Alcohol Awareness Month Twitter Chat hosted by NIAAA and the National Council on Alcoholism and Drug Dependence on April 28, 2015. Dr. Dunty served as the chat’s scientific expert.
Dr. Gary Murray participated in the 2015 Frank M. Norfleet Executive Forum on Health on April 30, 2015 at the University of Tennessee Health Science Center and the University of Memphis in Memphis Tennessee. The focus of this forum was “Vulnerability to Alcohol Use Disorders: Special Populations.”
NIAAA’s Division of Treatment and Recovery Research sponsored a research track at the American Psychiatric Association meeting, held May 16-20, 2015 in Toronto, Canada. The track was entitled “Advances in the Treatment of Alcohol and Co-occurring Psychiatric Disorders across Patient Populations and Settings.” The NIAAA-supported sessions featured in this research track included lectures, symposia, workshops, and forums by some of the world’s leading scientists in the alcohol research field. In addition to providing updates on new research, a number of sessions focused on the development of clinical knowledge and skills.
Dr. Antonio Noronha gave a presentation entitled “NIAAA Animal and Human Genetic Research Priorities” at the 17th Annual Genes, Brain and Behavior Meeting of the International Behavioral and Neural Genetics Society at Uppsala University in Sweden (May 19-22). Dr. Matthew Reilly from the Division of Neuroscience and Behavior co-chaired a symposium entitled “Epigenomic Mechanisms of Neuroadaptation and Neurodegeneration” at the same meeting.
Dr. Gary Murray met with staff from National Institute of Diabetes and Digestive and Kidney Diseases and the National Center for Health Statistics of the Centers for Disease Control and Prevention on May 21, 2015 in order to establish a collaborative Liver Elastography survey in a representative sample of the non-institutionalized population of the U.S.
Dr. Kenneth Warren was a speaker at the American Board on Addiction Medicine’s certification program ceremony on May 25, 2015, where he awarded certificates to program graduates.
Dr. Robert Freeman was a panel moderator for a symposium titled “Novel Interventions for HIV/AIDS Prevention” at the Society for Prevention Research’s (SPR) 2015 Annual Meeting, held in Washington, D.C., May 26-29, 2015. Dr. Freeman was also a member of the SPR Conference Organizing Committee. The panel featured talks by investigators from Johns Hopkins University, University of Maryland, and Hunter College on novel HIV risk reduction interventions among substance abusers.
Dr. Ralph Hingson was a panelist at the following two symposiums at the Society for Prevention Research’s 2015 Annual Meeting, held in Washington, D.C., May 26-29 2015: “Screening, Brief Intervention, and Referral to Treatment (SBIRT) for Drug Use in Health Care Settings: A Dialogue on the Evidence and Opportunity for Prevention” and “Marijuana Legalization in Washington State: Parental Attitudes and Prevention Messages.” He was also a co-author on a poster titled “Predicting Substance-Specific Impaired Driving in Emerging Adults.”
Dr. Michael Hilton co-edited Volume 36, Issue 1, of Alcohol Research: Current Reviews, titled “Alcohol Research and eHealth Technology.” The issue reports on the state of the science and future directions in electronic health (eHealth) technologies and their potential impact on alcohol epidemiology, prevention, and treatment. As an emerging and rapidly evolving transdisciplinary field, eHealth is poised to transform existing theories of behavioral change and models of behavioral health care.
Dr. Kathy Jung, NIAAA SBIR Coordinator represented NIAAA in establishing a collaboration with NIDA on a contract supplement to the NIDA BioRealm SBIR Phase II contract for the development of additional “Smokescreen” arrays for genotyping of addiction-related genetic samples. NIAAA will support the cost of arrays for alcohol-related genotype analysis and addiction-plus-alcohol related genotype analysis.
On June 19-20, 2015, NIAAA will sponsor through an R13 Conference grant, a satellite meeting, “Neuroimaging Mechanisms of Change in Psychotherapy for Addictive Behaviors,” in conjunction with the 2015 annual meeting of the Research Society on Alcoholism. This satellite will feature presentations by a number of NIAAA-supported investigators.
NIAAA and NIDA will hold Frontiers in Addiction Research: A Joint Mini-Convention in conjunction with the annual Society for Neuroscience meeting in Chicago on October 16, 2015. The focus of the mini-convention will be on the neurobiological and behavioral consequences of drug and alcohol use during development.
On December 5, 2015, NIAAA will sponsor a satellite meeting entitled, “NIAAA State-of-the-Science on Treating the Comorbidity of Alcohol Use Disorders and PTSD” prior to the 54th Annual Meeting of the American College of Neuropsychopharmacology (ACNP) in Hollywood, FL. The objective of this ANCP satellite meeting is to briefly review emerging new perspectives and highlight potential new opportunities for the development of novel treatments for the comorbidity of alcohol use disorders and PTSD.
The second “Annual Meeting for BRAIN Initiative Investigators” will be held December 10-11, 2015, in Bethesda, MD. This will be a multi-agency meeting with participation from investigators funded by NIH, NSF, DARPA and IARPA, including new awardees from NIH FY2015 RFAs. The overall goal of the meeting is to facilitate coordination and collaboration among the research teams, to highlight new findings, and to discuss future directions for the BRAIN Initiative.
Significance: A common functional polymorphism of the mu opioid receptor had previously been shown to predict response of patients with alcohol use disorders to naltrexone and to modulate reward. The findings show that the G carriers have a phenotype of a reduction in baseline mu opioid receptor availability, lower responses of endogenous opioids and dopamine to expectation of analgesia, and higher NEO-neuroticism scores. The results demonstrate that the A118G OPRM1 polymorphism contributes to interindividual variations in trait measures of pain and placebo responses and in the function of neurotransmitters responsive to pain and placebo.
ABSTRACT: Mu-opioid receptors (MOPRs) are critically involved in the modulation of pain and analgesia, and represent a candidate mechanism for the development of biomarkers of pain conditions and their responses to treatment. To further understand the human implications of genetic variation within the opioid system in pain and opioid-mediated placebo responses, we investigated the association between the functional single-nucleotide polymorphism (SNP) in the μ-opioid receptor gene (OPRM1), A118G, and psychophysical responses, personality traits, and neurotransmitter systems (dopamine (DA), opioid) related to pain and placebo analgesia. OPRM1 G carriers, compared with AA homozygotes, showed an overall reduction of baseline μ-opioid receptor availability in regions implicated in pain and affective regulation. In response to a sustained painful stimulus, we found no effect of A118G on pain-induced endogenous opioid release. Instead, AA homozygotes showed a blunted DA response in the nucleus accumbens (NAc) in response to the pain challenge. After placebo administration, G carriers showed more pronounced mood disturbances and lower placebo-induced μ-opioid system activation in the anterior insula (aINS), the amygdala (AMY), the NAc, the thalamus (THA), and the brainstem, as well as lower levels of DA D2/3 activation in the NAc. At a trait level, G carriers reported higher NEO-Neuroticism scores; a personality trait previously associated with increased pain and lower placebo responses, which were negatively correlated with baseline μ-opioid receptor availability in the aINS and subgenual anterior cingulate cortex (sgACC). Our results demonstrate that the A118G OPRM1 polymorphism contributes to interindividual variations in the function of neurotransmitters responsive to pain (endogenous opioid and dopamine), as well as their regulation through cognitive-emotional influences in the context of therapeutic expectations, the so-called placebo effect. These effects are relevant to human vulnerability to disease processes where these neurotransmitters have a role, such as persistent pain, mood, and substance use disorders, and responses to their treatments. (Peciña M, Love T, Stohler CS, Goldman D, Zubieta JK.
Neuropsychopharm, 2015 Mar;40(4):957-65. doi: 10.1038/npp.2014.272)
The contribution of rare and common variants in 30 genes to risk nicotine dependence
Significance: This study identified a panel of common and rare variants in 30 candidate genes for nicotine dependence (ND) (frequently comorbid with alcohol dependence) which were then genotyped in large datasets of European Americans and African Americans. Rare variants in a substantial proportion of these genes in both ethnicities significantly contributed to risk for ND and rare variants in two genes CHRNA9 (neuronal acetylcholine receptor subunit alpha-9) and GRIN3A (Glutamate [NMDA] receptor subunit 3A) were found in both the European American and African American data sets. This study has demonstrated a novel methodology for identifying the ‘hidden heritability’ of addictive disorders.
ABSTRACT: Genetic and functional studies have revealed that both common and rare variants of several nicotinic acetylcholine receptor subunits are associated with nicotine dependence (ND). In this study, we identified variants in 30 candidate genes including nicotinic receptors in 200 sib pairs selected from the Mid-South Tobacco Family population with equal numbers of African Americans (AAs) and European Americans (EAs). We selected 135 of the rare and common variants and genotyped them in the Mid-South Tobacco Case-Control (MSTCC) population, which consists of 3088 AAs and 1430 EAs. None of the genotyped common variants showed significant association with smoking status (smokers vs non-smokers), Fagerström Test for ND scores or indexed cigarettes per day after Bonferroni correction. Rare variants in NRXN1, CHRNA9, CHRNA2, NTRK2, GABBR2, GRIN3A, DNM1, NRXN2, NRXN3 and ARRB2 were significantly associated with smoking status in the MSTCC AA sample, with weighted sum statistic (WSS) P-values ranging from 2.42 × 10-3 to 1.31 × 10-4 after 106 phenotype rearrangements. We also observed a significant excess of rare nonsynonymous variants exclusive to EA smokers in NRXN1, CHRNA9, TAS2R38, GRIN3A, DBH, ANKK1/DRD2, NRXN3 and CDH13 with WSS P-values between 3.5 × 10-5 and 1 × 10-6. Variants rs142807401 (A432T) and rs139982841 (A452V) in CHRNA9 and variants V132L, V389L, rs34755188 (R480H) and rs75981117 (N549S) in GRIN3A are of particular interest because they are found in both the AA and EA samples. A significant aggregate contribution of rare and common coding variants in CHRNA9 to the risk for ND (SKAT-C: P=0.0012) was detected by applying the combined sum test in MSTCC EAs. Together, our results indicate that rare variants alone or combined with common variants in a subset of 30 biological candidate genes contribute substantially to the risk of ND. (Yang J, Wang S, Yang Z, Hodgkinson CA, Iarikova P, Ma JZ, Payne TJ, Goldman D, Li MD. Mol Psychiatry, 2014 Dec 2. doi: 10.1038/mp.2014.156. [Epub ahead of print])
Significance: Nearly one-third of adults in the United States have an AUD at some time in their lives, but only about 20 percent seek AUD treatment, according to new results from NIAAA’s 2012-2013 National Epidemiologic Survey on Alcohol and Related Conditions III (NESARC-III). Using diagnostic criteria set forth in the fifth edition of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM–5) in 2013, researchers found that 13.9 percent of adults met DSM-5 AUD criteria for the previous year, while 29.1 percent met AUD criteria at some time in their life. Only 19.8 percent of adults with lifetime alcohol use disorder sought treatment or help. Researchers also assessed NESARC III participants using the previous DSM-IV diagnostic criteria, and found large increases in DSM-IV alcohol use disorder rates compared with rates measured in the 2001-2002 NESARC survey.
Importance: National epidemiologic information from recently collected data on the new DSM-5 classification of alcohol use disorder (AUD) using a reliable, valid, and uniform data source is needed. Objective: To present nationally representative findings on the prevalence, correlates, psychiatric comorbidity, associated disability, and treatment of DSM-5 AUD diagnoses overall and according to severity level (mild, moderate, or severe). Design, Setting, and Participants: We conducted face-to-face interviews with a representative US noninstitutionalized civilian adult (≥18 years) sample (N = 36 309) as the 2012-2013 National Epidemiologic Survey on Alcohol and Related Conditions III (NESARC-III). Data were collected from April 2012 through June 2013 and analyzed in October 2014. Main Outcomes and Measures: Twelve-month and lifetime prevalences of AUD. Results: Twelve-month and lifetime prevalences of AUD were 13.9% and 29.1%, respectively. Prevalence was generally highest for men (17.6% and 36.0%, respectively), white (14.0% and 32.6%, respectively) and Native American (19.2% and 43.4%, respectively), respondents, and younger (26.7% and 37.0%, respectively) and previously married (11.4% and 27.1%, respectively) or never married (25.0% and 35.5%, respectively) adults. Prevalence of 12-month and lifetime severe AUD was greatest among respondents with the lowest income level (1.8% and 1.5%, respectively). Significant disability was associated with 12-month and lifetime AUD and increased with the severity of AUD. Only 19.8% of respondents with lifetime AUD were ever treated. Significant associations were found between 12-month and lifetime AUD and other substance use disorders, major depressive and bipolar I disorders, and antisocial and borderline personality disorders across all levels of AUD severity, with odds ratios ranging from 1.2 (95% CI, 1.08-1.36) to 6.4 (95% CI, 5.76-7.22). Associations between AUD and panic disorder, specific phobia, and generalized anxiety disorder were modest (odds ratios ranged from 1.2 (95% CI, 1.01-1.43) to 1.4 (95% CI, 1.13-1.67) across most levels of AUD severity. Conclusions and Relevance: Alcohol use disorder defined by DSM-5 criteria is a highly prevalent, highly comorbid, disabling disorder that often goes untreated in the United States. The NESARC-III data indicate an urgent need to educate the public and policy makers about AUD and its treatment alternatives, to destigmatize the disorder, and to encourage those who cannot reduce their alcohol consumption on their own, despite substantial harm to themselves and others, to seek treatment. (Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Pickering RP, Ruan WJ, Smith SM, Huang B, Hasin DS. JAMA Psychiatry. Published online June 03, 2015. doi: 10.1001/jamapsychiatry.2015.0584)
Significance: A substantial proportion of the U.S. adult population is at risk for alcohol-medication interactions. All individuals who drink, and particularly the elderly, should be educated about of the risks of combining alcohol with their medications.
BACKGROUND: The majority of Americans consume alcoholic beverages. Alcohol interacts negatively with numerous commonly prescribed medications. Yet, on a population level, little is known about use of alcohol-interactive (AI) prescription medications among drinkers. The purpose of our study was to determine the prevalence of AI prescription medication use among current drinkers in the U.S. population. METHODS: Data were from the National Health and Nutrition Examination Survey (NHANES 1999 to 2010); 26,657 adults aged ≥20 years had data on past year alcohol consumption and past month prescription medication use. Analyses were adjusted for covariates: age, race/ethnicity, education, marital status, and smoking. Statistical procedures accounted for survey stratification, clustering, and nonresponse. Analyses were weighted to be nationally representative. RESULTS: The unadjusted total prevalence of AI medication use was 42.8% (95% confidence interval [CI] 41.5 to 44.0). Among current drinkers, adjusted prevalence was 41.5% (CI 40.3 to 42.7). Among participants aged ≥65 total prevalence of AI medication use was 78.6% (CI 77.3 to 79.9) and adjusted prevalence among current drinkers was 77.8% (CI 75.7 to 79.7). The AI medications most commonly used by current drinkers were cardiovascular agents, central nervous system agents, and metabolic agents. CONCLUSIONS: Our results suggest that there could be substantial simultaneous exposure to alcohol and AI prescription medications in the U.S. population. Given the adverse health risks of combining alcohol with AI prescription medications, future efforts are needed to collect data to determine actual simultaneous prevalence. (Breslow RA, Dong C, White A. Alcohol Clin Exp Res, 2015 Feb;39(2):371-9. doi: 10.1111/acer.12633)
Restoration of Wnt/β-catenin signaling attenuates alcoholic liver disease progression in a rat model
Significance: Wnt/β-catenin signaling recently has been shown to promote inflammation and apoptosis, suggesting the hypothesis that activation of this signaling pathway may modulate alcoholic liver disease (ALD) progression. Using a rat model of chronic alcohol consumption, researchers showed that Wnt/β-catenin signaling plays a protective role in ALD progression via antagonizing Foxo3A-induced apoptosis, and that pharmacological activation of the Wnt/β-catenin signaling cascade attenuates ALD progression.
BACKGROUND & AIMS: Alcoholic liver disease (ALD) is characterized by the development of fatty liver, alcoholic hepatitis, fibrosis and cirrhosis. However, the underlying mechanism(s) associated with progression remains elusive. Pro-inflammatory cytokines have been implicated in ALD progression due to pro-apoptotic effects on hepatocytes. Wnt/β-catenin signaling recently has been shown to promote inflammation and apoptosis, suggesting that activation of this signaling pathway may modulate ALD progression. The current study was designed to test whether pharmacological activation of Wnt/β-catenin signaling altered ALD development and progression in a rat model. METHODS: Adult male Long Evans rats were fed with isocaloric liquid diets containing 0% or 37% ethanol for 8 weeks, and also treated with Wnt agonist during the last 3 weeks of the feeding regimen. Liver and blood samples were subjected to histology, TUNEL assay, immunoblot analysis, real-time quantitative PCR, and alanine transaminase (ALT) assay. RESULTS: Wnt/β-catenin signaling was negatively correlated with Foxo3A expression and reduced steatosis, cellular injury and apoptosis in ALD rats. Mutation experiments demonstrated that Foxo3A was critical for modulating these effects. Activation of Wnt/β-catenin signaling suppressed Foxo3A-induced apoptosis through up-regulation of serum/glucocorticoid regulated kinase 1 (SGK1). Moreover, pharmacological restoration of Wnt/β-catenin signaling reduced ALD progression in vivo. CONCLUSION: Wnt/β-catenin signaling plays a protective role in ALD progression via antagonizing Foxo3A-induced apoptosis and activation of the Wnt/β-catenin signaling cascade attenuates ALD progression. (Huang CK, Yu T, de la Monte SM, Wands JR, Derdak Z, Kim M. J Hepatol, 2015 Feb 24. pii: S0168-8278(15)00140-3. doi: 10.1016/j.jhep.2015.02.030. [Epub ahead of print])
Significance: The authors hypothesized that pharmacologic agents can be used to alter substrate specificity of related enzymes as replacements for defective isoforms in alcohol metabolism. This study demonstrates that when given with an aldehyde dehydrogenase 2 (ALDH2) specific activator, Alda-1, Alda-89 recruits aldehyde dehydrogenase 3A1 (ALDH3A1), a closely related enzyme, and this may be able to compensate for a loss of ability of ALDH2 to metabolize acetaldehyde. Alda-89 may be useful not only as an alcohol detoxifying drug, but as a cancer preventing strategy since ALDH3A1 is expressed in the mouth, upper airway, stomach and gut, all tissues prone to cancer development.
Correcting a genetic mutation that leads to a loss of function has been a challenge. One such mutation is in aldehyde dehydrogenase 2 (ALDH2), denoted ALDH2*2. This mutation is present in ∼0.6 billion East Asians and results in accumulation of toxic acetaldehyde after consumption of ethanol. To temporarily increase metabolism of acetaldehyde in vivo, we describe an approach in which a pharmacologic agent recruited another ALDH to metabolize acetaldehyde. We focused on ALDH3A1, which is enriched in the upper aerodigestive track, and identified Alda-89 as a small molecule that enables ALDH3A1 to metabolize acetaldehyde. When given together with the ALDH2-specific activator, Alda-1, Alda-89 reduced acetaldehyde-induced behavioral impairment by causing a rapid reduction in blood ethanol and acetaldehyde levels after acute ethanol intoxication in both wild-type and ALDH2-deficient, ALDH2*1/*2, heterozygotic knock-in mice. The use of a pharmacologic agent to recruit an enzyme to metabolize a substrate that it usually does not metabolize may represent a novel means to temporarily increase elimination of toxic agents in vivo. (Chen CH, Cruz LA, Mochly-Rosen D. Proc Natl Acad Sci USA, 2015;112:3074-9. doi: 10.1073/pnas.1414657112. Epub 2015 Feb 23)
NPY Signaling Inhibits Extended Amygdala CRF Neurons to Suppress Binge Alcohol Drinking
Significance: Binge alcohol drinking contributes to acute and chronic public health problems, and binge drinking by adolescents and college students contributes to alcohol use disorder and anxiety disorders. While binge alcohol drinking elevates corticotropin-releasing factor (CRF) activity and CRF signaling increases anxiety, neuropeptide Y (NPY) is known to reduce binge drinking and anxiety. This study reports that the anti-drinking effect of NPY is produced by enhancing the inhibition of CRF neurons in the bed nucleus of the stria terminalis (BNST), identifying a brain site at which stress modulates binge alcohol drinking.
Binge alcohol drinking is a tremendous public health problem because it leads to the development of numerous pathologies, including alcohol abuse and anxiety. It is thought to do so by hijacking brain systems that regulate stress and reward, including neuropeptide Y (NPY) and corticotropin-releasing factor (CRF). The central actions of NPY and CRF have opposing functions in the regulation of emotional and reward-seeking behaviors; thus, dysfunctional interactions between these peptidergic systems could be involved in the development of these pathologies. We used converging physiological, pharmacological and chemogenetic approaches to identify a precise neural mechanism in the bed nucleus of the stria terminalis (BNST), a limbic brain region involved in pathological reward and anxiety behaviors, underlying the interactions between NPY and CRF in the regulation of binge alcohol drinking in both mice and monkeys. We found that NPY Y1 receptor (Y1R) activation in the BNST suppressed binge alcohol drinking by enhancing inhibitory synaptic transmission specifically in CRF neurons via a previously unknown Gi-mediated, PKA-dependent postsynaptic mechanism. Furthermore, chronic alcohol drinking led to persistent alterations in Y1R function in the BNST of both mice and monkeys, highlighting the enduring, conserved nature of this effect across mammalian species. Together, these data provide both a cellular locus and signaling framework for the development of new therapeutics for treatment of neuropsychiatric diseases, including alcohol use disorders. (Pleil KE, Rinker JA, Lowery-Gionta EG, Mazzone CM, McCall NM, Kendra AM, Olson DP, Lowell BB, Grant KA, Thiele TE, Kash TL. Nature Neuroscience, 18:545-552. doi: 10.1038/nn.3972. Epub 2015 Mar 9)
Significance: The present study tests the hypothesis that alcohol exposure during adolescence impacts amygdala dependent functions such as anxiety in adulthood. The results of the study suggest that adolescent alcohol exposure causes persistent decreases in histone acetylation leading to lower expression of brain-derived neurotrophic factor (BDNF) and activity-regulated cytoskeleton-associated (Arc) protein genes paralleled by increased anxiety-like responses and increased ethanol drinking in adulthood. Administration of histone deacetylase (HDAC) 2 inhibitors during adolescent reverses the epigenetic and behavior changes.
Binge drinking is common during adolescence and can lead to the development of psychiatric disorders, including alcoholism in adulthood. Here, the role and persistent effects of histone modifications during adolescent intermittent ethanol (AIE) exposure in the development of anxiety and alcoholism in adulthood were investigated. Rats received intermittent ethanol exposure during post-natal days 28-41, and anxiety-like behaviors were measured after 1 and 24h of the last AIE. The effects of AIE on anxiety-like and alcohol-drinking behaviors in adulthood were measured with or without treatment with the histone deacetylase (HDAC) inhibitor, trichostatin A (TSA). Amygdaloid brain regions were collected to measure HDAC activity, global and gene-specific histone H3 acetylation, expression of brain-derived neurotrophic factor (BDNF) and activity-regulated cytoskeleton-associated (Arc) protein and dendritic spine density (DSD). Adolescent rats displayed anxiety-like behaviors after 24h, but not 1h, of last AIE with a concomitant increase in nuclear and cytosolic amygdaloid HDAC activity and HDAC2 and HDAC4 levels leading to deficits in histone (H3-K9) acetylation in the central (CeA) and medial (MeA), but not in basolateral nucleus of amygdala (BLA). Interestingly, some of AIE-induced epigenetic changes such as, increased nuclear HDAC activity, HDAC2 expression, and decreased global histone acetylation persisted in adulthood. In addition, AIE decreased BDNF exons I and IV and Arc promoter specific histone H3 acetylation that was associated with decreased BDNF, Arc expression and DSD in the CeA and MeA during adulthood. AIE also induced anxiety-like behaviors and enhanced ethanol intake in adulthood, which was attenuated by TSA treatment via normalization of deficits in histone H3 acetylation of BDNF and Arc genes. These novel results indicate that AIE induces long-lasting effects on histone modifications and deficits in synaptic events in the amygdala, which are associated with anxiety-like and alcohol drinking behaviors in adulthood. (Pandey SC, Sakharkar AJ, Tang L, and Zhang H. Neurobiol Dis, 2015 Mar 24. pii: S0969-9961(15)00091-1. doi: 10.1016/j.nbd.2015.03.019. [Epub ahead of print])
Significance: This study tests the hypothesis that alcohol exposure during adolescence impacts hippocampal functions in adulthood. The results of the study show that, in rats, adolescent intermittent alcohol exposure (AIE) decreased the threshold for long-term potentiation, making hippocampal neurons more easily excitable, an adolescent-specific phenotype that persists into adulthood. AIE also resulted in an increased number of dendritic spines with characteristics typical of immaturity, as well as an overall decrease in postsynaptic membrane proteins. These findings support the emerging hypothesis that adolescent alcohol exposure induces an array of neural changes that can manifest with immature-like characteristics into adulthood.
BACKGROUND: Human adolescence is a crucial stage of neurological development during which ethanol (EtOH) consumption is often at its highest. Alcohol abuse during adolescence may render individuals at heightened risk for subsequent alcohol abuse disorders, cognitive dysfunction, or other neurological impairments by irreversibly altering long-term brain function. To test this possibility, we modeled adolescent alcohol abuse (i.e., intermittent EtOH exposure during adolescence [AIE]) in rats to determine whether adolescent exposure to alcohol leads to long-term structural and functional changes that are manifested in adult neuronal circuitry. METHODS: We specifically focused on hippocampal area CA1, a brain region associated with learning and memory. Using electrophysiological, immunohistochemical, and neuroanatomical approaches, we measured post-AIE changes in synaptic plasticity, dendritic spine morphology, and synaptic structure in adulthood. RESULTS: We found that AIE-pretreated adult rats manifest robust long-term potentiation, induced at stimulus intensities lower than those required in controls, suggesting a state of enhanced synaptic plasticity. Moreover, AIE resulted in an increased number of dendritic spines with characteristics typical of immaturity. Immunohistochemistry-based analysis of synaptic structures indicated a significant decrease in the number of co-localized pre- and postsynaptic puncta. This decrease is driven by an overall decrease in 2 postsynaptic density proteins, PSD-95 and SAP102. CONCLUSIONS: Taken together, these findings reveal that repeated alcohol exposure during adolescence results in enduring structural and functional abnormalities in the hippocampus. These synaptic changes in the hippocampal circuits may help to explain learning-related behavioral changes in adult animals preexposed to AIE. (Risher ML, Fleming RL, Risher WC, Miller KM, Klein RC, Wills T, Acheson SK, Moore SD, Wilson WA, Eroglu C, Swartzwelder HS. Alcohol Clin Exp Res, 2015 Apr 27. Doi: 10.1111/acer.12725. [Epub ahead of print])
Significance: KCNN3, which encodes KCa2.3 channel, has been identified in multiple alcohol- and drug-related quantitative trait loci (QTL) and gene sets. This study, together with previous findings, provides genomic, behavioral, and physiological evidence that activity of KCNN3 negatively modulates voluntary and excessive alcohol consumption and that the KCa2.3 channel represents a potential target for the treatment of alcohol and drug addiction.
Small-conductance Ca2+-activated K+ (KCa2) channels control neuronal excitability and synaptic plasticity, and have been implicated in substance abuse. However, it is unknown if genes that encode KCa2 channels (KCNN1-3) influence alcohol and drug addiction. In the present study, an integrative functional genomics approach shows that genetic datasets for alcohol, nicotine, and illicit drugs contain the family of KCNN genes. Alcohol preference and dependence QTLs contain KCNN2 and KCNN3, and Kcnn3 transcript levels in the nucleus accumbens (NAc) of genetically diverse BXD strains of mice predicted voluntary alcohol consumption. Transcript levels of Kcnn3 in the NAc negatively correlated with alcohol intake levels in BXD strains, and alcohol dependence enhanced the strength of this association. Microinjections of the KCa2 channel inhibitor apamin into the NAc increased alcohol intake in control C57BL/6J mice, while spontaneous seizures developed in alcohol-dependent mice following apamin injection. Consistent with this finding, alcohol dependence enhanced the intrinsic excitability of medium spiny neurons in the NAc core and reduced the function and protein expression of KCa2 channels in the NAc. Altogether, these data implicate the family of KCNN genes in alcohol, nicotine, and drug addiction, and identify KCNN3 as a mediator of voluntary and excessive alcohol consumption. KCa2.3 channels represent a promising novel target in the pharmacogenetic treatment of alcohol and drug addiction. (Padula AE, Griffin WC 3rd, Lopez MF1, Nimitvilai S, Cannady R, McGuier NS, Chesler EJ, Miles MF, Williams RW, Randall PK, Woodward JJ, Becker HC, Mulholland PJ. Neuropsychopharm, 2015 Feb 9. doi: 10.1038/npp.2015.42 [Epub ahead of print])
Heterogeneity of Alcohol Use Disorder: Understanding Mechanisms to Advance Personalized Treatment
Significance: Alcohol Use Disorder (AUD) is a heterogeneous disorder for which alcohol researchers have developed various typologies to define the different phenotypes. Continued progress in neurobiology and genetics may facilitate the identification of biologically-based AUD subtypes and the selection of treatments to target those subtypes. The authors propose a framework for classifying AUDs into major functional domains and identifying constructs and measures within those domains that could be used to better characterize and tailor treatments to individuals with AUD.
The development of an alcohol addiction domain criteria-based framework to conceptualize research on AUD that probes the sources of the disorder could serve to organize and advance our understanding of alcohol addiction. This model would organize constructs and measures within the domains of AUD and help to define the constructs for addictive behaviors more generally, delving into brain function, neural circuitry, genes, and gene–environment interactions. Identifying the major domains underlying AUD and how the profile of vulnerability to each domain varies among individuals, and over time, not only will be vital to understand the heterogeneity of the disorder, but will also enable us to tailor treatment effectively to the individual. This will substantially advance the field of personalized medicine, and foster the translation of findings from basic research into practical, clinical applications. These research accomplishments will, undoubtedly, play a prominent role in health care over the next decade and bring alcohol treatment into mainstream medicine, a goal that the alcohol research community has been working toward for many years. (Litten R, Ryan M, Falk D, Reilly M, Fertig J and Koob G. Alcohol Clin Exp Res, 39(4): 579-584. doi: 10.1111/acer.12669)
Significance: No current pharmacotherapies to date have been shown to decrease both alcohol use and posttraumatic stress disorder (PTSD) symptom severity. Prazosin, an alpha-1 adrenoreceptor antagonist, offers promise in this arena insofar as previous studies have demonstrated that prazosin decreases drinking in animal models and PTSD symptoms in humans. This study found that prazosin decreased alcohol consumption but surprisingly not PTSD symptoms in patients with comorbid alcohol dependence and PTSD disorder. Since prazosin has shown efficacy for PTSD alone in other studies, additional research is needed, particularly exploring different dosing regimens of prazosin as well as other α-1 adrenergic antagonists in this understudied population.
Background: Posttraumatic stress disorder (PTSD) and alcohol dependence (AD) commonly co-occur and are associated with greater symptom severity and costs than either disorder alone. No pharmacologic interventions have been found to decrease both alcohol use and PTSD symptom severity relative to matched placebo. Prazosin, an alpha-1 adrenoreceptor antagonist, has demonstrated the efficacy of reducing PTSD and AD symptoms among individuals with one or the other disorder and may be useful in addressing comorbid PTSD/AD. Methods: Prazosin and matched placebo were compared in the context of an outpatient 6-week double-blind randomized controlled pilot trial involving 30 individuals with comorbid PTSD/AD. Medication was titrated to 4 mg q AM, 4 mg q PM and 8 mg qhs by the end of week 2. Participants in both conditions received 5 medical management sessions. Information regarding alcohol use, craving, and PTSD was gathered daily using a telephone interactive voice response system. Results: Participants randomized to prazosin had a greater reduction in percent days drinking per week and percent days heavy drinking per week between baseline and week 6 than did placebo participants. No significant differences were detected within or between groups in change from weeks 1 to 6 in total PTSD symptoms. Participants in the prazosin condition reported drowsiness on significantly more days than those in the placebo condition. Conclusions: Consistent with the extant research evaluating medications for comorbid PTSD/AD, the current evaluation of prazosin also found decreased alcohol consumption but no medication effect on PTSD symptomatology. (Simpson T, Malte C, Dietel B, Tell D, Pocock I, Lyons R, Varon D, Raskind M and Saxon A. Alcohol Clin Exp Res, 39(5): 808-8117. doi: 10.1111/acer.12703. Epub 2015 Apr 1)
Significance: Ethyl glucornide (EtG) is an alcohol biomarker that holds considerable promise as a potential clinical research and alcohol treatment outcome. Findings highlight that a low 200 ng/ml EtG cut-off level is recommended for assessing recent alcohol use. EtG immunoassay appears to be a potentially valuable tool that may enhance the accuracy of alcohol use assessment.
Background: Ethyl glucuronide (EtG) is an alcohol biomarker with potential utility as a clinical research and alcohol treatment outcome. Debate exists regarding the appropriate cutoff level for determining alcohol use, particularly with the EtG immunoassay. This study determined the EtG immunoassay cutoff levels that most closely correspond to self-reported drinking in alcohol-dependent outpatients. Methods: Eighty adults with alcohol dependence and mental illness, taking part in an alcohol treatment study, provided urine samples 3 times per week for up to 16 weeks (1,589 samples). Self-reported drinking during 120 hours prior to each sample collection was assessed. Receiver operating characteristic analyses were conducted to assess the ability of the EtG immunoassay to detect self-reported alcohol use across 24- to 120-hour time periods. Sensitivity and specificity of EtG immunoassay cutoff levels was compared in 100 ng/ml increments (100 to 500 ng/ml) across 24 to 120 hours. Results: Over half (57%) of the 1,589 samples indicated recent alcohol consumption. The EtG immunoassay closely corresponded to self-reported drinking from 24 (area under the curve [AUC] = 0.90, 95% confidence interval [CI]: 0.88, 0.92) to 120 hours (AUC = 0.88, 95% CI: 0.87, 0.90). When cutoff levels were compared across 24 to 120 hours, 100 ng/ml had the highest sensitivity (0.93 to 0.78) and lowest specificity (0.67 to 0.85). Relative to 100 ng/ml, the 200 ng/ml cutoff demonstrated a reduction in sensitivity (0.89 to 0.67), but improved specificity (0.78 to 0.94). The 300, 400, and 500 ng/ml cutoffs demonstrated the lowest sensitivity (0.86 to 0.33) and highest specificity (0.86 to 0.97) over 24 to 120 hours. Conclusions: For detecting alcohol use for >24 hours, the 200 ng/ml cutoff level is recommended for use as a research and clinical outcome. (Lowe J, McDonell M, Leickly E, Angelo F, Vilardaga R, McPherson S, Srebnik D, Roll J and Ries R. Alcohol Clin Exp Research, 39(5): 905-910; doi: 10.1111/acer.12699. Epub 2015 Apr 10)
Number of Drinks to “Feel a Buzz” by HIV Status and Viral Load in Men
Significance: HIV infected men reported a lower mean number of drinks to “feel a buzz” compared to uninfected men. After adjustment for body mass index and other factors, HIV-infected individuals with a detectable viral load required greater than a quarter of a drink less to feel a buzz compared to uninfected individuals (approximately 3.5 vs 3.1 drinks). Future research should examine whether this increased sensitivity among HIV positive individuals is due to increased blood alcohol concentrations or decreased tolerance for similar levels. Providers should consider these findings as they screen for alcohol use and counsel patients regarding the impact of alcohol on HIV infection.
The impact of HIV and its treatment on the effects of alcohol remain unclear. Blood alcohol concentrations have been noted to be higher in HIV infected individuals prior to antiretroviral initiation. Our goal was to compare number of drinks to “feel a buzz or high” among HIV infected and uninfected men, stratified by viral load (VL) suppression. Data includes 1478 HIV infected and 1170 uninfected men in the veterans aging cohort study who endorsed current drinking. Mean (SD) number of drinks to feel a buzz was 3.1 (1.7) overall. In multivariable analyses, HIV infected men reported a lower mean number of drinks to feel a buzz compared to uninfected men (coef = −14 for VL < 500; −34 for VL ≥ 500; p ≤ .05). Men with HIV, especially those with a detectable VL, reported fewer drinks to feel a buzz. Future research on the relationship between alcohol and HIV should consider the role of VL suppression. (McGinnis KA, Fiellin DA, Tate JP, Cook RL, Braithwaite RS, Bryant KJ, Edelman EJ, Gordon AJ, Kraemer KL, Maisto SA, Justice AC. Aids and Behavior, 17 April 2015.
Significance: While decreasing overall, risk of hospitalization remains higher among HIV positive individuals than uninfected individuals and is strongly influenced by the presence or absence of an Alcohol Related Diagnosis (ARD). In particular, gastrointestinal, liver, endocrine, neurologic, and non-AIDS cancer admissions increased among those with an ARD. Using effective comprehensive treatment programs to treat ARDs and their associated conditions, including psychiatric disease, could reduce inpatient utilization and overall morbidity in both HIV positive and uninfected patients.
Individuals with HIV infection are living substantially longer on antiretroviral therapy, but hospitalization rates continue to be relatively high. We do not know how overall or diagnosis-specific hospitalization rates compare between HIV-infected and uninfected individuals or what conditions may drive hospitalization trends. Hospitalization rates among United States Veterans were calculated and stratified by HIV serostatus and principal diagnosis disease category. Because alcohol-related diagnoses (ARD) appeared to have a disproportional effect, we further stratified our calculations by ARD history. A multivariable Cox proportional hazards model was fitted to assess the relative risk of hospitalization controlling for demographic and other comorbidity variables. From 1997 to 2011, 46,428 HIV-infected and 93,997 uninfected patients were followed for 1,497,536 person-years. Overall hospitalization rates decreased among HIV-infected and uninfected patients. However, cardiovascular and renal insufficiency admissions increased for all groups while gastrointestinal and liver, endocrine, neurologic, and non-AIDS cancer admissions increased among those with an alcohol-related diagnosis. After multivariable adjustment, HIV-infected individuals with an ARD had the highest risk of hospitalization (hazard ratio 3.24, 95 % CI 3.00, 3.49) compared to those free of HIV infection and without an ARD. Still, HIV alone also conferred increased risk (HR 2.08, 95 % CI 2.04, 2.13). While decreasing overall, risk of all-cause hospitalization remains higher among HIV-infected than uninfected individuals and is strongly influenced by the presence of an ARD. (Rentsch C, Tate JP, Akgün KM, Crystal S, Wang KH, Ryan Greysen S, Wang EA, Bryant KJ, Fiellin DA, Justice AC, Rimland D. AIDS Behav. 2015 Feb 26. [Epub ahead of print]
Wearable Alcohol Biosensor Competition

NIAAA is holding a competition to create a better wearable alcohol biosensor and has been conducting a range of outreach activities to publicize the project. Targeting biotechnology media, academia, and professional audiences through social media, press interviews, and outreach to potential applicants, NIAAA’s efforts have already generated a number of stories, including a news item on the Engineering in Medicine & Biology Society website and placement on the MedGadget blog.
The biosensor will aid researchers, clinicians, therapists and individuals by providing more accurate data on how much an individual is drinking. Presently, the biosensor bracelets commonly used in the criminal justice system are effective but cumbersome and only take readings every 30 minutes. A working prototype and supporting data is due December 1, 2015. The winner of the challenge prize will be awarded $200,000. Further details are available here.
Press and Publications Activities:
- Recent News Media Interviews: Dr. Koob has conducted more than 100 interviews with the press since he became the director of NIAAA. He recently has been interviewed by a variety of national and international news outlets on timely topics related to NIAAA’s research and its impact on treatment and prevention of alcohol misuse and alcohol use disorders. These include interviews with print outlets such as USA Today, U.S. News & World Report, NPR Health News, Nature, Glamour, and radio and television interviews with Fox 5 News at 6pm (NYC), and the Dr. Drew Pinsky Radio Show.

-
- CNN Visit and Interview: CNN Chief Medical Correspondent and neurosurgeon, Dr. Sanjay Gupta (middle) met with NIAAA Director Dr. George Koob (right) at NIAAA’s bar-like lab when he visited NIH on March 25, 2015, to deliver the annual J. Edward Rall Cultural Lecture. Dr. Gupta hopes to use information from this meeting and subsequent discussions for a future CNN story about NIAAA’s research. Dr. Lorenzo Leggio (left), also participated in the visit. Through the NIH and NIAAA Communications offices, Dr. Gupta was offered several options for his clinical center visit and selected only this NIAAA lab for a personal tour and interview. Dr. Leggio uses the virtual bar to explore alcohol triggers and to test potential new medications.
-
HBO Documentary: Dr. Koob and Dr. Deidra Roach were recently filmed for an HBO documentary that explores problem drinking; Dr. Koob continues to serve as an advisor to the show’s producers.
Publication StatisticsAs of April 1, there were 29,699 subscribers to the Alcohol Alert; 28,937 to Alcohol Research: Current Reviews; 18,925 to the NIAAA Spectrum; and 18,566 to receive general information.
Press Releases
NIH study finds alcohol use disorder on the increase (June 3, 2015)
NIAAA recognizes Alcohol Awareness Month 2015 (April 2, 2015)
Study defines brain and behavioral effects of teen binge drinking (April 2, 2015)
NIH holds competition to create better wearable alcohol biosensor (March 16, 2015)
NIH-funded scientists identify brain site for stress role in binge alcohol drinking (March 10, 2015)
Dr. Gary Wand to deliver 7th Annual Jack Mendelson Honorary Lecture at the National Institutes of Health (March 5, 2015)
Molecule hijacks enzyme to boost alcohol metabolism (February 23, 2015)
The February 2015 issue of NIH Research Matters featured a recap of the January news release: “NIH study reveals many Americans at risk for alcohol-medication interactions.”
Partnerships, Outreach, & Public Liaison Activities:Alcohol Awareness Month
In honor of Alcohol Awareness Month, NIAAA issued a press release and produced a series of graphics on the harms of excessive drinking that were tweeted throughout April. The month culminated with a Twitter chat held by NIAAA and co-hosted by the National Council on Alcohol and Drug Dependence (NCADD). The chat, “Alcohol and Your Health,” was the largest NIAAA chat to date, with messages about liver function, underage drinking, and low-risk drinking limits reaching an estimated 2.1 million accounts. Dr. William Dunty served as the scientific expert for the chat. An archived version is available here.
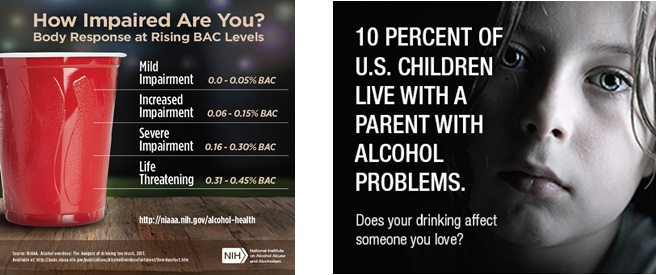
Seasonal Outreach – St. Patrick’s DayNIAAA also produced graphics to share on social media for St. Patrick’s Day. The images were tweeted by addiction specialist and host of HLN’s ‘Dr. Drew on Call,’ Dr. Drew Pinsky; ABC News Chief Dr. Richard Besser; WRC-TV news anchor Doreen Gentzler; and actress Mackenzie Phillips from TV’s “One Day at a Time.” Organizations including Mothers Against Drunk Driving, the Centers for Disease Control and Prevention, the National Institute on Drug Abuse, the Department of Health and Human Services Office on Women’s Health, and Stanford University also retweeted. Overall, the two St. Patrick’s Day graphics and tweets had an estimated reach of 6.4 million people based on total number of followers and re-tweets.
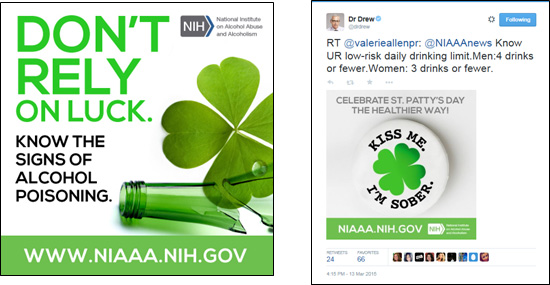
Seasonal Outreach – Super Bowl
People Magazine placed NIAAA’s Super Bowl graphic in regular rotation on their website, free of charge, during the week leading up to the Super Bowl. Dr. Richard Besser, Chief Health and Medical Editor of ABC News, tweeted another NIAAA Super Bowl graphic to his 46,800 followers.
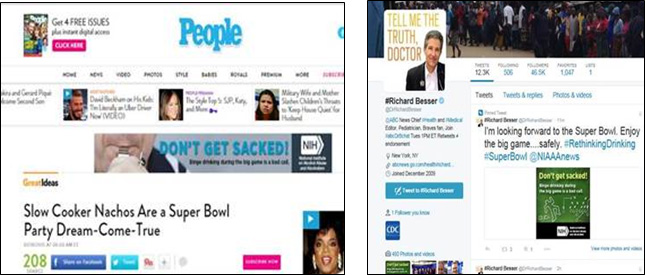
Partnerships: Since February 2015, the Communications and Public Liaison Branch has initiated new collaborative projects with a number of new and existing liaison groups:
- NIAAA presented three workshops at the Community Anti-Drug Coalitions of America’s (CADCA) National Leadership Forum on February 3, 2015, focusing on the new NIAAA treatment publication, college drinking, and NIAAA’s research priorities.
- Articles on NIAAA’s treatment publication appeared in the online newsletter of the American Society of Addiction Medicine.
- NIAAA received approval to produce an instructive webinar on the CollegeAIM from PaperClip, a company that produces webinars for college administrators.
- NIAAA also has ongoing collaborative activities with the National Organization on Fetal Alcohol Syndrome and Community of Concern.
- NIAAA is supporting the efforts of the Substance Abuse Librarians and Information Specialists (SALIS) to digitize a library of substance abuse literature and make it available online to the public. NIAAA provided a large selection of books to SALIS for digitization, as well as funding to help support the labor costs involved in scanning and uploading these books.

