NIAAA Director's Report on Institute Activities to the 140th Meeting of the National Advisory Council on Alcohol Abuse and Alcoholism
Table of Contents
- NIAAA BUDGET
- LEGISLATIVE NEWS
- COLLABORATIVE RESEARCH ON ADDICTION AT NIH UPDATE
- DIRECTOR'S ACTIVITIES
- STAFF TRANSITIONS
- HONORS AND AWARDS
- NEW NOTICE OF FUNDING OPPORTUNITIES
- NOTABLE NIAAA STAFF ACTIVITIES
- WHAT'S AHEAD
- NIH RESEARCH HIGHLIGHTS
- NIAAA COMMUNICATIONS ACTIVITIES
FY 2015
The NIAAA is currently closing out fiscal year (FY) 2015 to coincide with the end of the federal fiscal year calendar which ends September 30, 2015. In FY 2015, NIH received a total of $30.3 billion, an increase of $150 million above the FY 2014 level.
The FY 2015 appropriation for NIAAA provided $447.2 million. This represented an increase of $1.4 million or 0.3% over the FY 2014 level. NIAAA estimates that it will support a total of 676 research project grants (RPG) in FY 2015, including 152 competing awards, compared to 686 RPGs and 180 competing awards in FY 2014.
FY 2016
As discussed in the June Director’s Report to Council, President Obama submitted to Congress his FY 2016 budget request for all federal agencies on February 2, 2015 – the FY 2016 President’s Budget. Included in the President’s request is a proposed FY 2016 budget for the NIH of $31.3 billion, a $1 billion increase over the FY 2015 level. The NIAAA budget request for FY 2016 is $459.8 million, an increase of $12.6 million over the FY 2015 level.
The FY 2016 appropriations bill for the NIH budget is still pending in Congress. As a result, NIH anticipates beginning FY 2016 under a Continuing Resolution (CR). A CR is legislation that allows federal operations and programs to continue at current spending levels when formal appropriations bills have not been signed into law by the end of a fiscal year. Following is the current status of FY 2016 NIH appropriations activity in the House and Senate:
House Action: On June 24, 2015, the House Appropriations Committee approved a FY 2016 Labor-Health and Human Services-Education funding bill that would provide NIH with $31.2 billion, which is $1.1 billion more than the FY 2015 level. For NIAAA, the bill would provide $456 million, which is $8.6 million more than the FY 2015 level.
Senate Action: On June 25, 2015, the Senate Appropriations Committee approved its version of the FY 2016 Labor-Health and Human Services-Education funding bill. For NIH, the budget level proposed by the Senate Committee is $32.0 billion, an increase of $2 billion above the FY 2015 level. This is the largest proposed increase to the NIH budget since the end of the budget doubling in FY 2003. For NIAAA, the proposed budget level in the bill is $469.4 million, which is $22.2 million more than the FY 2015 level.
Although these funding bills passed successfully though their respective committees, they have yet to be considered by the full legislature in both the House and Senate.
FY 2017
Preliminary work on the budget for FY 2017 has begun. After intermediate stages of review, the President’s budget request will be presented to Congress in February 2016, at which time it will become available to the public.
| FY 2015 Enacted |
FY 2016 President's Budget |
|||
|---|---|---|---|---|
| MECHANISM | Number | Amount | Number | Amount |
| Research Projects | ||||
| Noncompeting | 501 | $189,337 | 491 | $186,684 |
| Administrative Supplements | (24) | 1,269 | (24) | 1,269 |
| Competing | 152 | 51,595 | 176 | 59,120 |
| Subtotal, RPGs | 653 | 242,201 | 667 | 247,073 |
| SBIR/STTR | 23 | 10,445 | 37 | 11,889 |
| Research Centers | ||||
| Specialized/Comprehensive | 18 | 28,446 | 704 | 28,200 |
| Clinical Research | - | - | - | - |
| Biotechnology | - | - | - | - |
| Comparative Medicine | - | - | - | - |
| Res. Centers in Minority Instit. | - | - | - | - |
| Subtotal, Centers | 18 | 28,446 | 17 | 28,200 |
| Other Research | ||||
| Research Careers | 90 | 14,017 | 93 | 14,000 |
| Cancer Education | - | - | ||
| Cooperative Clinical Research | 1 | 7,272 | 1 | 7,180 |
| Biomedical Research Support | - | - | ||
| Minority Biomed. Research Support | 340 | |||
| Other | 44 | 15,268 | 46 | 15,000 |
| Subtotal, Other Research | 135 | 36,897 | 140 | 36,180 |
| Total Research Grants | 829 | 317,989 | 861 | 323,342 |
| Training | ||||
| Individual | 106 | 4233 | 99 | 4500 |
| Institutional | 174 | 8,456 | 175 | 8,700 |
| Total, Training | 174 | 8,456 | 175 | 8,700 |
| Research & Develop. Contracts | 67 | 36,535 | 69 | 42,552 |
| (SBIR/STTR) | (2) | (1,601) | (4) | (1,100) |
| Intramural Research | 109 | 49,496 | 109 | 49,991 |
| Res. Management & Support | 128 (4) |
30,444 (10) |
128 | 30,748 |
| Total, NIAAA | $447,153 | $459,833 |
||
COLLABORATIVE RESEARCH ON ADDICTION AT NIH UPDATE
All participating NIH Institutes and Centers (ICs) have signed off on the funding plan for the Adolescent Brain Cognitive Development (ABCD) Study, and notices of grant award will go out in the next few days. The awards are to be made in FY 2015.
NIAAA’s Director, Dr. George Koob, made a number of notable presentations during the last three months:
- He provided opening remarks and a report from NIAAA to commence the 2015 Annual Meeting of the Research Society on Alcoholism (RSA).
- He gave the opening plenary at the Annual Meeting of the National Hispanic Science Network (NHSN) in San Antonio, Texas. NIAAA hopes to expand interest in Hispanic-focused alcohol research and is pleased that the meeting featured two invited alcohol-related symposia in addition to Dr. Koob’s plenary.
- He spoke at the opening of the joint meeting of the International Drug Abuse Research Society (IDARS) and the Asia-Pacific Society for Alcohol and Addiction Research (APSAAR). The meeting was held in Sydney Australia, in mid-August. Dr. Koob’s presentation was titled, “Dark Side Medications for Treating Addiction.”
- He spoke at the Victoria University Wellington School of Psychology in Wellington, New Zealand, on August 26, 2015. The subject was “Addiction as a Stress Surfeit Disorder.”
- He gave a plenary lecture on August 29, 2015, titled, “Neurobiology of Addiction: Cerberus Revisited” at the 33rd International Australasian Winter Conference on Brain Research in Queenstown, New Zealand.

Vicki Buckley joined the Office of Resource Management in May 2015, as the Deputy Executive Officer for NIAAA. Prior to joining NIAAA, Vicki served as the Deputy Executive Officer/Acting Executive Officer for the National Eye Institute (NEI) since January, 2013. Prior to NEI, she worked at the National Institute on Mental Health (NIMH) from 1999 to 2013, serving in numerous administrative roles including over three years as the Chief Administrative Officer for the NIMH Intramural Research Program. Vicki has an extensive background in NIH administration including financial management, acquisitions, property management, human resources, and policy and management analysis. Vicki earned a B.S. in Health Care Management from Southern Illinois University, and a Master’s in Business Administration from Mt. Saint Mary’s University.
Mr. Keith Lamirande left NIAAA on August 7, 2015, having accepted an offer to serve as Executive Officer at the National Center for Advancing Translational Sciences (NCATS). Keith had an illustrious 14-year career at NIAAA, in positions of increasing administrative and management responsibility, from Budget Analyst, to Deputy and then Budget Officer, to Deputy Executive Officer, and finally Executive Officer/Associate Director for Administration as well as Deputy Ethics Counselor. He was widely acclaimed at NIAAA and NIH for his leadership and mentorship skills.
Ms. Charlene Patrick departed NIAAA in July to join the Administrative Management Branch in the Division of Intramural Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), where she serves as Lead Administrative Officer. Charlene served in various extramural and intramural roles during her tenure at NIAAA.
Ms. Fanny Rio Spears, who served as a Staff Assistant to the Deputy Director of NIAAA, left NIAAA in August to pursue her career as an Executive Assistant with the Texas Heart Institute in Houston, Texas.
Ms. Tamica Wilkerson departed NIAAA in August for NCATS. In her new role at NCATS, she will serve as the Administrative Officer to the Executive Office. NIAAA appreciates her six years of service to the Institute in various administrative roles.
Dr. David Goldman received the RSA Distinguished Researcher Award and the RSA Seventh Annual Ting-Kai Li, M.D. Plenary Lecture Award in June 2015. The title of his talk was: “The Genetics of Alcoholism: The Interface of Genes, Environment and Choice.”
Nine NIAAA intramural fellow researchers won NIH Fellows Award for Research Excellence (FARE). Of 25 applicants from NIAAA, 36 percent won an award. The overall NIH award rate was 26.5 percent. The winners (with their mentors in parentheses) are:
- Dr. Jessica Chancey (Dr. Dave Lovinger)
- Dr. Resat Cinar (Dr. George Kunos)
- Dr. Joshua Gowin (Dr. Vijay Ramchandani)
- Dr. Lindsay Halladay (Dr. Andrew Holmes)
- Mr. Yong He (Dr. Bin Gao)
- Dr. Teresa Ramirez (Dr. Bin Gao)
- Dr. Ming-Jiang Xu (Dr. Bin Gao)
- Dr. Jia Yan (Dr. Vijay Ramchandani)
- Dr. Zhou Zhou (Dr. Bin Gao)
Dr. Anita Bechtholt and Ms. Megan Ryan, M.B.A., received an Office of Human Resources Group Award for their roles in organizing NIAAA’s research track at the American Psychiatric Association meeting, creating the NIAAA Employee Awards Program, and organizing the Lunch & Learn series.
Dr. Jessica Chancey, Mr. David Kupferschmidt, and Dr. Shana Augustin received Society for Neuroscience (SfN) travel awards to the International Brain Research Organization 2016 meeting.
Dr. Mehdi Farokhnia was the National Institute on Drug Abuse (NIDA) travel award winner to 2015 International Society of Addiction Medicine conference.
NEW NOTICE OF FUNDING OPPORTUNITIES (NOFOs)
The following RFAs and PAs were issued by NIAAA:
RFA-AA-16-001: Limited Competition: Consortia for HIV/AIDS and Alcohol-Related Research Trials (CHAART) Project (Collaborative U01). This proposed research initiative is aligned with the research priorities set forth in the Trans-NIH Plan for HIV-Related Research.
RFA-AA-16-002: Limited Competition: Consortia for HIV/AIDS and Alcohol-Related Research Trials (CHAART) Administrative Core (U24). The overall goal of this .NOFO is to provide administrative support for advancing operations or implementation research in the context of alcohol and HIV/AIDS as set forth in the Trans-NIH Plan for HIV-Related Research.
RFA-AA-16-003: Limited Competition: Consortia for HIV/AIDS and Alcohol-Related Research Trials (CHAART) Resource Core (U24). This proposed research initiative is aligned with the priorities set forth in the Trans-NIH Plan for HIV-Related Research.
PA-15-294, PA-15-295, PA-15-296: Screening and Brief Alcohol Interventions in Underage and Young Adult Populations (R21, R01, R03, respectively). The objective of these NOFOs is to encourage research on screening and brief interventions to prevent and/or reduce alcohol use and alcohol-related harms among underage and young adult populations.
PA-15-299, PA-15-300, PA-15-301: Alcohol Use Disorder (AUD): Behavioral Treatment, Services and Recovery Research (R01, R03, R21, respectively). These NOFOs encourage grant applications from institutions/organizations that propose to support research on behavioral treatment for AUD; organizational, financial, and management factors that facilitate or inhibit the delivery of services for AUD; and phenomenon of recovery from AUD.
NIAAA is participating in the following NOFOs:
RFA-EB-15-006 (National Institute of Biomedical Imaging and Bioengineering): BRAIN: Theories, Models and Methods for Analysis of Complex Data from the Brain (R01). This NOFO solicits new theories, computational models, and statistical methods to derive understanding of brain function from complex neuroscience data. Approaches could include the creation of new theories, ideas, and conceptual frameworks to organize/unify data and infer general principles of brain function; new computational models to develop testable hypotheses and design/drive experiments; and new mathematical and statistical methods to support or refute a stated hypothesis about brain function, and/or assist in detecting features in complex brain data. It is expected that the approaches developed under this NOFO will be made widely available to the neuroscience research community for their use and modification.
RFA-CA-15-017 (National Cancer Institute (NCI)): Big Data to Knowledge (BD2K) Development of Software Tools and Methods for Biomedical Big Data in Targeted Areas of High Need (U01). The purpose of this BD2K NOFO is to solicit development of software tools and methods in the three topic areas of data privacy, data repurposing, and applying metadata, all as part of the overall BD2K initiative. While this NOFO is intended to foster new development, submissions consisting of significant adaptations of existing methods and software are also invited.
RFA-MH-16-725 (NIMH): BRAIN Initiative: Technology Sharing and Propagation (R03). This NOFO encourages the dissemination of new technologies and new data analysis techniques beyond the laboratory or company where they originated. It provides funds to enable the incorporation of new technologies or data analysis techniques into research programs that further the aims of the BRAIN initiative.
PAR-15-280 (NIA), PAR-15-281 (NIA), PAR-15-282 (NIA): Multidisciplinary Studies of HIV/AIDS and Aging (R01, R03, R21, respectively). These NOFOs invite applications proposing to study HIV infection, HIV-associated conditions, HIV treatment, and/or biobehavioral or social factors associated with HIV/AIDS in the context of aging and/or in older adults. Research approaches of interest include clinical translational, observational, and intervention studies in domestic and international settings.
PAR-15-286 (NICHD): Pre-application: Opportunities for Collaborative Research at the NIH Clinical Center (X02). This NOFO encourages X02 pre-applications for Opportunities for Collaborative Research at the NIH Clinical Center. The X02 pre-application is the recommended (not required) first step in the application process for the companion NOFO (PAR-15-287). Potential applicants should read both NOFOs. Investigators whose X02 pre-applications are meritorious, can be accommodated by the resources of the NIH Clinical Center and the relevant intramural program, and align with the research missions of the participating NIH Institutes, will be notified of the opportunity to submit a U01 application under PAR-15-287.
PAR-15-287 (NICHD): Opportunities for Collaborative Research at the NIH Clinical Center (U01). The goal of this program is to support collaborative translational research projects aligned with NIH efforts to enhance the translation of basic biological discoveries into clinical applications that improve health. It encourages high quality science demonstrating the potential to result in understanding an important disease process or lead to new therapeutic interventions, diagnostics, or prevention strategies within the research interests and priorities of the participating NIH ICs.
PA-15-322 (NCI): Research Supplements to Promote Re-Entry into Biomedical and Behavioral Research Careers (Admin Supp). The NIH and the U.S. Centers for Disease Control and Prevention hereby notify Program Director(s)/Principal Investigator(s) (PD(s)/PI(s)) holding specific types of research grants (activity codes listed above) that funds are available for administrative supplements to improve the diversity of the research workforce by recruiting and supporting students, postdoctorates, and eligible investigators from groups that have been shown to be underrepresented in health-related research. This supplement opportunity is also available to PD(s)/PI(s) of research grants who are or become disabled and need additional support to accommodate their disability in order to continue to work on the research project. Administrative supplements must support work within the scope of the original project.
PA-15-329 (NCI) Administrative Supplements for Research on Sexual and Gender Minority (SGM) Populations (Admin Supp). The NIH Office of the Director announces the availability of administrative supplements to expand existing research to focus on Sexual and Gender Minority (SGM) health. SGM populations include, but are not limited to, lesbian, gay, bisexual, and transgender people, and individuals with differences or disorders of sexual development (sometimes referred to as “intersex” or as specific diagnoses). This trans-NIH effort, which involves multiple ICs and Offices from across NIH, is intended to encourage investigation in this underrepresented growing field of research. To increase our collective understanding of the broad range of the health needs of SGM populations, the supplement will focus on areas of specific research interest beyond HIV/AIDS, including, but not limited to studies on increased disease risk, behavioral and social health, approaches to personalized medicine, access to care, reproductive and sexual development, and resilience.
NOTABLE NIAAA STAFF ACTIVITIES -- JUNE - SEPTEMBER 2015
Dr. Ralph Hingson gave a number of presentations since the last Council meeting. The first presentation, “Preventing Drug-Impaired Driving and Overdoses: Lessons from Alcohol-Impaired Driving,” was given at the Mothers Against Drunk Driving’s Driving Under the Influence of Drugs Task Force Meeting, in Washington, D.C., on June 22, 2015. This talk explored ways in which research on alcohol-impaired driving could help guide future research on drug-impaired driving and reduce and prevent drug-impaired driving. He also presented on the topic “New Research since the Surgeon General’s Call to Action to Prevent and Reduce Underage Drinking” at the Community Anti-Drug Coalitions of America’s 2015 Mid-Year Training Institute in Indianapolis, Indiana, on August 5, 2015. This talk outlined new research on trends in and consequences of underage drinking and interventions to prevent and reduce underage drinking that have emerged since the 2007 Call to Action.
The “Improving Health Through Translational Alcohol Research” issue of Alcohol Research: Current Reviews was released on June 29, 2015. Dr. Antonio Noronha and Dr. Edie Sullivan served as scientific review editors. Maureen Gardner and Dr. Jennifer Hobin served as editors in chief.
Dr. Lorenzo Leggio spoke on “Model of Team Science - Collaboration between academia, government and industry supported by NCATS” at the American Association of Colleges of Pharmacy Annual Meeting, National Harbor, Maryland, July 13, 2015.
Dr. Dionne Godette gave a presentation titled, “Using alcohol epidemiology data to inform preventive intervention research: Epidemiological measurement methodology considerations for prevention research,” at the NIH Chronic Disease Capacity Building workshop in Needham’s Point, Barbados, July 20–24, 2015. She also facilitated a roundtable titled, “Evidence-based behavioral and social interventions addressing tobacco and alcohol outcomes.” The presentation and roundtable also focused on the associations between excessive/risky drinking patterns and chronic non‐communicable diseases and conditions (e.g., diabetes, obesity, cardiovascular diseases and cancer and alcohol, tobacco, and other drugs addiction).
NIAAA provided support through R13 conference grants for the joint meeting of the Fourth APSAAR (August 18–21) and Fifth IDARS meeting. Dr. Kenneth Warren gave the opening plenary at a special fetal alcohol spectrum disorders (FASD)-focused day. Dr. Peggy Murray made a presentation and chaired a panel discussion on policy and legal issues in FASD at which Council member Judge Linda Chezem presented on issues with FASD in the U.S. Judicial system. Dr. Antonio Noronha chaired a session on Preventing Drug Seeking and Relapse in which Dr. George Koob and Dr. Andrew Holmes made presentations.
Gregory Bloss organized and co-chaired a workshop on “Economics of Prevention” on August 27–28 on the NIH campus in Bethesda, Maryland. The workshop was co-sponsored by the NIH Common Fund Health Economics Program and the NIH Office of Disease Prevention and Health Promotion.
Drs. Lindsey Grandison, Ellen Witt, and Anita Bechtholt, took the lead in organizing a trans-NIH workshop titled, “Resilience Concept Development Workshop,” held September 16, 2015, in Rockville, Maryland. This workshop, sponsored by the Office of Behavioral and Social Science Research Opportunities Network (OppNET), brought together leaders in the resilience research field, to identify the gaps, opportunities and priorities for future resilience research. The outcomes of this workshop will provide a basis for a future OppNET NOFO on resilience.
NIAAA Staff Activities at the 2015 Annual Meeting of the RSA, San Antonio, Texas, June 20–24:
- Drs. Brett Hagman and Robert Huebner co-organized a symposium titled “Current Trends and Future Directions in Screening and Assessment for DSM-5 Alcohol Use Disorder.”
- Dr. Mike Hilton organized and chaired a symposium on “Alcohol, Marijuana, and Policy.” Mr. Gregory Bloss served as discussant for the session, which featured presentations by four current NIAAA grantees.
- Dr. Mary Lee and Dr. Lorenzo Leggio organized and co-chaired a symposium titled, “Role of oxytocin in addiction: beyond “love story.” Dr. Lee also served as a speaker (“Importance of Oxytocin and Dopamine in Addiction: A Translational Approach”) and Dr. Leggio served as the discussant.
- Drs. Gary Murray and Svetlana Radaeva with Dr. Pranoti Mandrekar of University of Massachusetts, organized a symposium titled, “Translational Approaches in Alcohol Hepatitis: Concepts to Drug Development.” Dr. Radaeva presented introductory remarks and Dr. Murray provided discussion and overview.
- Dr. Peggy Murray was co-organizer and chair of an international symposium on Prevention of FASD that included presentations from NIAAA-funded work in Russia and South Africa, an Italian public awareness program that has been implemented in several European cities, and the World Health Organization (WHO) Project to Develop Guidelines for Addiction Treatment of Pregnant Women.
- Dr. Abbas Parsian, co-organized a symposium titled, “Genomics of Alcoholism: What Can We Learn Through Sequencing?” The focus of this symposium was on next-generation sequencing and how these techniques can be used to understand alcoholism and related phenotypes.
- Dr. Antonio Noronha co-organized a symposium titled, “Emerging Role of MicroRNAs in Alcohol-related Behaviors.” This symposium discussed advances in identifying alcohol-induced changes in miRNA target gene networks in brain that are correlated with alcohol-related behaviors and toxicity. Dr. Noronha also presented at another symposium titled, “Myelin in Alcohol and Drug Abuse: Chicken or the Egg?,” and gave introductory remarks at the inaugural meeting of “Neuroimaging Mechanisms of Change in Psychotherapy for Addictive Behaviors,” a satellite held prior to the RSA meeting.
- Drs. H. Joe Wang and Kathy Jung, together with Dr. Bin Gao of the Laboratory of Liver Disease, co-organized and co-chaired a symposium titled, “Neutrophils In Alcohol-Induced Organ Damage: Functional Consequences And Clinical Implications”.
- Dr. Matthew Reilly organized a satellite workshop titled, “Genomic and Computational Approaches for Biomarker and Drug Discovery.” The purpose of this workshop was to bring together lead scientists for one of the NIH Common Fund’s programs called “Library of Integrated Network-based Cellular Signatures” (LINCS) and scientists from the alcohol research community to explore how LINCS resources can facilitate identification of druggable targets and novel and/or repurposed compounds for the treatment of alcohol dependence.
- Drs. Mark Egli and Soundar Regunathan participated in a roundtable discussion titled, “Sex and the lab: a discussion about the NIH initiative to balance sex in cell and animal studies.” Dr. Regunathan gave opening remarks and Dr. Egli presented an update on NIH’s planned policy to require consideration of sex as a biological variable in research involving animal subjects.
- Drs. Robert Huebner, Daniel Falk, and Brett Hagman provided the NIAAA update at the 11th Annual Satellite Session Research on Mechanisms of Behavior Change.
- Dr. Kathy Jung gave a presentation titled, “NIAAA-Supported Research Overview” at the “NIAAA-Supported Research: A Grantsmanship Workshop.”
- Dr. Raye Litten presented at two symposia. His talks were titled, “Validating Clinical Relevance of Potential Drinking Endpoints in Clinical Trials” and “New Research Advances in Development and Implementation of Ethanol Sensors and Biomarkers of Ethanol Consumption.”
- Dr. Changhai Cui presented the introduction to the symposium titled, “Ethanol Effects on the Developing Brain: the Role and Consequences of Glial Activation and Neuroinflammatory Events.” Her talk provided an overview of the role of glial activation in neuroinflammatory events, including how multiple factors impact ethanol’s action on microglial activities in FASD and AUD.
- Dr. Gary Murray presented the introduction to the symposium on “Mechanisms of Alcohol-Induced Tumor Promotion,” organized by Dr. Jia Luo, University of Kentucky, Lexington, Kentucky.
Several key NIAAA staff presented at the 15th European Society for Biomedical Research on Alcoholism (ESBRA) Congress in Valencia, Spain, September 12-15, 2015:
- Dr. Peggy Murray gave a keynote presentation on “The Adolescent Brain and Cognitive Development (ABCD) study: significance, challenges and opportunities.” She was introduced by Dr. Kenneth Warren.
- Dr. Antonio Noronha co-chaired and gave introductory remarks at a symposium, and presented on “Persistent epigenetic marks—DNA methylation: Why this matters in Alcoholism.” Dr. Noronha also co-chaired and gave introductory remarks at the Congress’s symposium on “Consequences of adolescent alcohol abuse: human and animal studies.”
- Dr. Kenneth Warren co-chaired the symposium on advances in FASD.
- Dr. Gary Murray, with Dr. Helmut Seitz, University of Heidelberg, co-organized and co-chaired a symposium on alcoholic liver disease. Dr. Murray also served as discussant at the symposium “New Insights into Post-Translational Protein Modifications in the Initiation and Progression of Alcohol-Induced Liver Injury.”
Drs. Brett Hagman and Robert Huebner will be providing an update on the Division of Treatment and Recovery Research’s screening and brief intervention portfolio at this year’s International Network for Brief Interventions for Alcohol and Other Drugs conference in Atlanta, Georgia, September 23–25, 2015.
In October 2015, Dr. Ralph Hingson will present his poster titled, “Traffic Risk Behaviors among Emerging Adults Who Drive after Drinking, Marijuana Use, or Other Drug Use,” at the 2015 Global Alcohol Policy Conference (GAPC), sponsored by the WHO and other organizations. The conference will be in Edinburgh, Scotland. Dr. Hingson will also represent the U.S. Government at the WHO’s Second Meeting of the Coordinating Council for the implementation of the WHO Global Strategy to reduce the harmful use of alcohol, which will be held in conjunction with GAPC.
On October 17, 2015, NIAAA and NIDA will sponsor a mini-convention in conjunction with the Annual Meeting of the SfN, Chicago, Illinois, titled, “Frontiers in Addiction Research: Neurobiological and Behavioral Consequences of Drug and Alcohol Use during Development.” This one-day event featuring leading experts in their field will focus on the effects of alcohol and substance use on the developing brain from the cognitive/behavioral to the genetic and molecular level.
On October 21, 2015, a symposium titled, “Adolescent alcohol exposure: Long-term neurobiological and behavioral consequences” will be held at the Annual Meeting of the SfN, Chicago, Illinois. The symposium will discuss recent findings on the neurobiological and behavioral consequences of alcohol use during adolescence that persists into adulthood in animal models.
On December 5, 2015, NIAAA will sponsor a satellite meeting titled, “NIAAA State-of-the-Science on Treating the Comorbidity of AUD and [Post-Traumatic Stress Disorder] PTSD” prior to the 54th Annual Meeting of the American College of Neuropsychopharmacology (ACNP) in Hollywood, Florida. The objective of this ACNP satellite meeting is to briefly review emerging new perspectives and highlight potential new opportunities for the development of novel treatments for the comorbidity of AUD and PTSD.
The second “Annual Meeting for BRAIN Initiative Investigators” will be held December 10–11, 2015, in Bethesda, Maryland. This will be a multi-agency meeting with participation from investigators funded by NIH, the National Science Foundation, the Defense Advanced Research Projects Agency, and the Intelligence Advanced Research Projects Agency, including new awardees from NIH FY 2015 RFAs. The overall goal of the meeting is to facilitate coordination and collaboration among the research teams, to highlight new findings, and to discuss future directions for the BRAIN Initiative.
The 2016 Gordon Research Conference (GRC) on Alcohol and the Nervous System will be held February 7–12, 2016, at Hotel Galvez, Galveston, Texas. This conference will cover a broad range of studies at the molecular, cellular, circuit/systems and behavioral level, with particular emphasis on multidisciplinary work and innovative approaches.
Significance: Alcohol-induced apoptosis of neural crest cells (NCC) is thought to contribute to the facial anomalies seen with prenatal alcohol exposure (PAE). This report shows that the microRNA miR-125b protects against apoptosis by blocking the expression of known mediators of apoptosis and that alcohol disrupts this protection by reducing miR-125b levels in both cultured NCC and embryos. Furthermore, injection of miR-125b into alcohol-exposed mouse embryos was shown to prevent apoptosis and improve embryo growth. Collectively, these findings define a mechanism by which alcohol impairs fetal development and suggests the possibility that a miR-125b-based intervention could diminish the harm caused by PAE to the fetus.
ABSTRACT: MicroRNAs are a class of small noncoding RNAs that have been implicated in regulation of a broad range of cellular and physiologic processes, including apoptosis. The objective of this study is to elucidate the roles of miR-125b in modulating ethanol-induced apoptosis in neural crest cells (NCCs) and mouse embryos. We found that treatment with ethanol resulted in a significant decrease in miR-125b expression in NCCs and in mouse embryos. We also validated that Bcl-2 antagonist killer 1 (Bak1) and p53-upregulated modulator of apoptosis (PUMA) are the direct targets of miR-125b in NCCs. In addition, over-expression of miR-125b significantly reduced ethanol-induced increase in Bak1 and PUMA protein expression, caspase-3 activation, and apoptosis in NCCs, indicating that miR-125b can modulate ethanol-induced apoptosis by the regulation of Bcl-2 and p53 pathways. Furthermore, microinjection of miR-125b mimic resulted in a significant increase in miR-125b expression and a decrease in the protein expression of Bak1 and PUMA in ethanol-exposed mouse embryos. Up-regulation of miR-125b also significantly reduced ethanol-induced caspase-3 activation and diminished ethanol-induced growth retardation in mouse embryos. This is the first demonstration that miR-125b can prevent ethanol-induced apoptosis and that microinjection of miRNA mimic can prevent ethanol-induced embryotoxicity. (Chen X, Liu J, Feng WK, Wu X, Chen SY. Exp Neurol, 2015 May 27;271:104-111. doi: 10.1016/j.expneurol.2015.04.026.)
Significance: Using a sheep model, these investigators demonstrated that third trimester binge-drinking reduces fetal plasma levels of glutamine and related amino acids and, furthermore, impedes fetal growth, including fetal brain growth. Both the fetal amino acid disturbances and growth restriction were mitigated by administering glutamine to the pregnant sheep, suggesting that glutamine infusion might be a beneficial intervention in human pregnancies known to involve significant alcohol exposure.
ABSTRACT: Prenatal alcohol exposure is known to cause fetal growth restriction and disturbances in amino acid bioavailability. Alterations in these parameters can persist into adulthood and low birth weight can lead to altered fetal programming. Glutamine has been associated with the synthesis of other amino acids, an increase in protein synthesis and it is used clinically as a nutrient supplement for low birth weight infants. The aim of this study was to explore the effect of repeated maternal alcohol exposure and L-glutamine supplementation on fetal growth and amino acid bioavailability during the third trimester-equivalent period in an ovine model. Pregnant sheep were randomly assigned to four groups, saline control, alcohol (1.75-2.5 g/kg), glutamine (100 mg/kg, three times daily) or alcohol + glutamine. In this study, a weekend binge drinking model was followed where treatment was done 3 days per week in succession from gestational day (GD) 109-132 (normal term ~147). Maternal alcohol exposure significantly reduced fetal body weight, height, length, thoracic girth and brain weight, and resulted in decreased amino acid bioavailability in fetal plasma and placental fluids. Maternal glutamine supplementation successfully mitigated alcohol-induced fetal growth restriction and improved the bioavailability of glutamine and glutamine-related amino acids such as glycine, arginine, and asparagine in the fetal compartment. All together, these findings show that L-glutamine supplementation enhances amino acid availability in the fetus and prevents alcohol-induced fetal growth restriction. (Sawant OB, Wu G, Washburn SE. Amino Acids, 2015 Jun;47(6):1183-92. doi: 10.1007/s00726-015-1945-x.)
Brain Development in Heavy-Drinking Adolescents
Significance: This study used magnetic resonance imaging to examine brain gray and white matter volume trajectories in adolescents who transitioned to heavy drinking compared to those who did not. Longitudinal analyses detected an acceleration in the typical decline in volume of neocortical areas and smaller increases in white matter volume in adolescents who started drinking heavily. The findings provide further evidence that heavy drinking during adolescence alters the trajectory of brain development.
OBJECTIVE: Heavy alcohol use during adolescence may alter the trajectory of normal brain development. The authors measured within-subject changes in regional brain morphometry over longer intervals and in larger samples of adolescents than previously reported and assessed differences between adolescents who remained nondrinkers and those who drank heavily during adolescence as well as differences between the sexes. METHOD: The authors examined gray and white matter volume trajectories in 134 adolescents, of whom 75 transitioned to heavy drinking and 59 remained light drinkers or nondrinkers over roughly 3.5 years. Each underwent MRI scanning two to six times between ages 12 and 24 and was followed for up to 8 years. The volumes of the neocortex, allocortex, and white matter structures were measured using atlas-based parcellation with longitudinal registration. Linear mixed-effects models described differences in trajectories of heavy drinkers and nondrinkers over age; secondary analyses considered the contribution of other drug use to identified alcohol use effects. RESULTS: Heavy-drinking adolescents showed accelerated gray matter reduction in cortical lateral frontal and temporal volumes and attenuated white matter growth of the corpus callosum and pons relative to nondrinkers. These results were largely unchanged when use of marijuana and other drugs was examined. Male and female drinkers showed similar patterns of development trajectory abnormalities. CONCLUSIONS: Longitudinal analysis enabled detection of accelerated typical volume decline in frontal and temporal cortical volumes and attenuated growth in principal white matter structures in adolescents who started to drink heavily. These results provide a call for caution regarding heavy alcohol use during adolescence, whether heavy drinking is the sole cause or one of several in these alterations in brain development. (Squeglia LM, Tapert SF, Sullivan EV, Jacobus J, Meloy MJ, Rolfing T, Pfefferbaum A. Am J Psychiatry, 2015, 172(6):532-42).
Girk3 Gates Activation of the Mesolimbic Dopaminergic Pathway by Ethanol
Significance: G protein-gated inwardly rectifying potassium (GIRK) channels regulate neuronal excitability. This study shows that genetic deletion of the GIRK3 subunit prevents alcohol activation of the mesolimbic dopaminergic pathway and enhances binge-like drinking, suggesting that GIRK3 is a critical gatekeeper of ethanol incentive salience and a potential target for the treatment of excessive ethanol consumption.
G protein-gated inwardly rectifying potassium (GIRK) channels are critical regulators of neuronal excitability and can be directly activated by ethanol. Constitutive deletion of the GIRK3 subunit has minimal phenotypic consequences, except in response to drugs of abuse. Here we investigated how the GIRK3 subunit contributes to the cellular and behavioral effects of ethanol, as well as to voluntary ethanol consumption. We found that constitutive deletion of GIRK3 in knockout (KO) mice selectively increased ethanol binge-like drinking, without affecting ethanol metabolism, sensitivity to ethanol intoxication, or continuous-access drinking. Virally mediated expression of GIRK3 in the ventral tegmental area (VTA) reversed the phenotype of GIRK3 KO mice and further decreased the intake of their wild-type counterparts. In addition, GIRK3 KO mice showed a blunted response of the mesolimbic dopaminergic (DA) pathway to ethanol, as assessed by ethanol-induced excitation of VTA neurons and DA release in the nucleus accumbens. These findings support the notion that the subunit composition of VTA GIRK channels is a critical determinant of DA neuron sensitivity to drugs of abuse. Furthermore, our study reveals the behavioral impact of this cellular effect, whereby the level of GIRK3 expression in the VTA tunes ethanol intake under binge-type conditions: the more GIRK3, the less ethanol drinking. (Herman MA, Sidhu H, Stouffer DG, Kreifeldt M, Le D, Cates-Gatto C, Munoz MB, Roberts AJ, Parsons LH, Roberto M, Wickman K, Slesinger PA, Contet C. Proceedings of the National Academy of Sciences 112:7091-7096.)
Significance: This study applies systems biology algorithms originally developed and consistently shown to identify causal molecular targets for cancer treatment to alcohol dependence. The computational approaches were applied to a rat model of dependence and protracted abstinence. A novel druggable genomic target was identified, the glucocorticoid receptor gene (Nr3c1), that acts as a causal “Master Regulator” of the gene expression signature produced by protracted abstinence. This correlation between protracted abstinence and Nr3c1 was causally validated in vivo; the Nr3c1 antagonist mifepristone selectively decreased dependent, excessive, alcohol self-administration in rats. A recently published human laboratory pilot study on mifepristone supports the rat model results.
BACKGROUND: A systems biology approach based on the assembly and interrogation of gene regulatory networks, or interactomes, was used to study neuroadaptation processes associated with the transition to alcohol dependence at the molecular level. RESULTS: Using a rat model of dependent and non-dependent alcohol self-administration, we reverse engineered a global transcriptional regulatory network during protracted abstinence, a period when relapse rates are highest. We then interrogated the network to identify master regulator genes that mechanistically regulate brain region-specific signatures associated with dependent and non-dependent alcohol self-administration. Among these, the gene coding for the glucocorticoid receptor was independently identified as a master regulator in multiple brain regions, including the medial prefrontal cortex, nucleus accumbens, central nucleus of the amygdala, and ventral tegmental area, consistent with the view that brain reward and stress systems are dysregulated during protracted abstinence. Administration of the glucocorticoid antagonist mifepristone in either the nucleus accumbens or ventral tegmental area selectively decreased dependent, excessive, alcohol self-administration in rats but had no effect on non-dependent, moderate, alcohol self-administration. CONCLUSIONS: Our study suggests that assembly and analysis of regulatory networks is an effective strategy for the identification of key regulators of long-term neuroplastic changes within specific brain regions that play a functional role in alcohol dependence. More specifically, our results support a key role for regulatory networks downstream of the glucocorticoid receptor in excessive alcohol drinking during protracted alcohol abstinence. (Repunte-Canonigo V, Shin W, Vendruscolo LF, Lefebvre C, van der Stap L, Kawamura T, Schlosburg JE, Alvarez M, Koob GF, Califano A, Sanna PP. Genome Biol. 2015 Feb 2;16(1):68. [Epub ahead of print])
Significance: This study links a polymorphism in the gene for brain-derived neurotrophic factor to increased risk of compulsive alcohol intake. It underscores the contribution of a genetic factor to AUD and identifies a potential therapeutic target for the treatment of compulsive alcohol drinking.
BACKGROUND: The valine 66 to methionine (Met) polymorphism within the brain-derived neurotrophic factor (BDNF) sequence reduces activity-dependent BDNF release and is associated with psychiatric disorders in humans. Alcoholism is one of the most prevalent psychiatric diseases. Here, we tested the hypothesis that this polymorphism increases the severity of alcohol abuse disorders. METHODS: We generated transgenic mice carrying the mouse homolog of the human Met66BDNF allele (Met68BDNF) and used alcohol-drinking paradigms in combination with viral-mediated gene delivery and pharmacology. RESULTS: We found that Met68BDNF mice consumed excessive amounts of alcohol and continued to drink despite negative consequences, a hallmark of addiction. Importantly, compulsive alcohol intake was reversed by overexpression of the wild-type valine68BDNF allele in the ventromedial prefrontal cortex of the Met68BDNF mice or by systemic administration of the tropomyosin receptor kinase B agonist, LM22A-4. CONCLUSIONS: Our findings suggest that carrying this BDNF allele increases the risk of developing uncontrolled and excessive alcohol drinking that can be reversed by directly activating the BDNF receptor, tropomyosin receptor kinase B. Importantly, this work identifies a potential therapeutic strategy for the treatment of compulsive alcohol drinking in humans carrying the Met66BDNF allele. (Warnault V, Darcq E, Morisot N, Phamluong K, Wilbrecht L, Massa SM, Longo FM4, Ron D. Biol Psychiatry online. 2015 Jun 12. pii: S0006-3223(15)00481-3)
Significance: Previous research indicates that the hormone glucagon-like peptide-1 (GLP-1) regulates appetite and food intake, and that GLP-1 receptor (GLP-1R) activation attenuates the reinforcing properties of alcohol in rodents. This paper presents data from four human genetic association studies suggesting a role of a genetic variant of the glucagon-like peptide-1 receptor (GLP-1R) in alcohol dependence. In an additional translational study, GLP-1R agonism significantly reduced alcohol consumption in a mouse model of alcohol dependence. These convergent findings suggest that GLP-1R may represent a novel pharmacotherapy target for AUD.
The hormone glucagon-like peptide-1 (GLP-1) regulates appetite and food intake. GLP-1 receptor (GLP-1R) activation also attenuates the reinforcing properties of alcohol in rodents. The present translational study is based on four human genetic association studies and one preclinical study providing data that support the hypothesis that GLP-1R may have a role in the pathophysiology of alcohol use disorder (AUD). Case-control analysis (N = 908) was performed on a sample of individuals enrolled in the National Institute on Alcohol Abuse and Alcoholism (NIAAA) intramural research program. The Study of Addiction: Genetics and Environment (SAGE) sample (N = 3803) was used for confirmation purposes. Post hoc analyses were carried out on data from a human laboratory study of intravenous alcohol self-administration (IV-ASA; N = 81) in social drinkers and from a functional magnetic resonance imaging study in alcohol-dependent individuals (N = 22) subjected to a Monetary Incentive Delay task. In the preclinical study, a GLP-1R agonist was evaluated in a mouse model of alcohol dependence to demonstrate the role of GLP-1R for alcohol consumption. The previously reported functional allele 168Ser (rs6923761) was nominally associated with AUD (P = 0.004) in the NIAAA sample, which was partially replicated in males of the SAGE sample (P = 0.033). The 168 Ser/Ser genotype was further associated with increased alcohol administration and breath alcohol measures in the IV-ASA experiment and with higher BOLD response in the right globus pallidus when receiving notification of outcome for high monetary reward. Finally, GLP-1R agonism significantly reduced alcohol consumption in a mouse model of alcohol dependence. These convergent findings suggest that the GLP-1R may be an attractive target for personalized pharmacotherapy treatment of AUD (Suchankova P, Yan J, Schwandt ML, Stangl BL, Caparelli EC, Momenan R, Jerlhag E, Engel JA, Hodgkinson CA, Egli M, Lopez MF, Becker HC, Goldman D, Heilig M, Ramchandani VA, Leggio L. Transl Psychiatry. 2015;5:e583)
Effects of Varenicline on Neural Correlates of Alcohol Salience in Heavy Drinkers
Significance: This study demonstrates the effects of varenicline on activation of brain regions associated with motivation and incentive salience for alcohol reward in heavy drinkers. The attenuation of striato-cortico-limbic responses to cues signaling alcohol reward by varenicline may underlie its clinical effectiveness in reducing alcohol consumption and its potential utility in pharmacotherapy for AUD.
BACKGROUND: Preclinical and emerging clinical evidence indicates that varenicline, a nicotinic partial agonist approved for smoking cessation, attenuates alcohol seeking and consumption. Reductions of alcohol craving have been observed under varenicline treatment and suggest effects of the medication on alcohol reward processing, but this hypothesis remains untested. METHODS: In this double-blind, placebo-controlled randomized experimental medicine study, 29 heavy drinkers underwent a functional magnetic resonance imaging scan after 2 weeks of varenicline (2mg/d) or placebo administration. During functional magnetic resonance imaging, participants performed the Alcohol-Food Incentive Delay task, where they could earn points for snacks or alcohol. At baseline and after 3 weeks of medication, participants underwent intravenous alcohol self-administration sessions in the laboratory. RESULTS: During the functional magnetic resonance imaging scan, participants in the varenicline group (N=17) reported lower feelings of happiness and excitement on subjective mood scales when anticipating alcohol reward compared with the placebo group (N=12). Linear mixed effects analysis revealed that anticipation of alcohol reward was associated with significant blood oxygen level dependent activation of the ventral striatum, amygdala, and posterior insula in the placebo group; this activation was attenuated in the varenicline group. The varenicline group showed no difference in intravenous alcohol self-administration relative to the placebo group for either session. Participants with higher insula activation when anticipating alcohol reward showed higher alcohol self-administration behavior across groups. CONCLUSIONS: Our findings suggest that varenicline decreases blood oxygen level dependent activation in striato-cortico-limbic regions associated with motivation and incentive salience of alcohol in heavy drinkers. This mechanism may underlie the clinical effectiveness of varenicline in reducing alcohol intake and indicates its potential utility as a pharmacotherapy for alcohol use disorders. (Vatsalya V, Gowin JL, Schwandt ML, Momenan R, Coe MA, Cooke ME, Hommer DW, Bartlett S, Heilig M, Ramchandani VA. Int J Neuropsychopharmacol. 2015 doi: 10.1093/ijnp/pyv068. [Epub ahead of print])
Significance: The α1-blocker doxazosin reduced alcohol drinking and craving in alcoholic patients with high density family history of alcoholism, while no effect was found in those with low family history density of alcoholism. This study suggests that doxazosin may be effective selectively in alcoholic patients with significant family history of alcoholism.
Evidence suggests that the norepinephrine system represents an important treatment target for alcohol dependence (AD) and the α1 -blocker prazosin may reduce alcohol drinking in rodents and alcoholic patients. The α1 -blocker doxazosin demonstrates a more favorable pharmacokinetic profile than prazosin, but has never been studied for AD. A double-blind placebo-controlled randomized clinical trial was conducted in AD individuals seeking outpatient treatment. Doxazosin or matched placebo was titrated to 16 mg/day (or maximum tolerable dose). Drinks per week (DPW) and heavy drinking days (HDD) per week were the primary outcomes. Family history density of alcoholism (FHDA), severity of AD and gender were a priori moderators. Forty-one AD individuals were randomized, 30 (doxazosin = 15) completed the treatment phase and 28 (doxazosin = 14) also completed the follow-up. There were no significant differences between groups on DPW and HDD per week. With FHDA as a moderator, there were significant FHDA × medication interactions for both DPW (pcorrected = 0.001, d = 1.18) and HDD (pcorrected = 0.00009, d = 1.30). Post hoc analyses revealed that doxazosin significantly reduced alcohol drinking in AD patients with high FHDA and by contrast increased drinking in those with low FHDA. Doxazosin may be effective selectively in AD patients with high FHDA. This study provides preliminary evidence for personalized medicine using α1 -blockade to treat AD. However, confirmatory studies are required (Kenna GA, Haass-Koffler CL, Zywiak WH, Edwards SM, Brickley MB, Swift RM, Leggio L. Addict Biol. 2015 Jun 2. [Epub ahead of print])
Significance: The quality of the relationship between a therapist and his or her client can make a significant contribution to recovery from substance use disorders. Researchers examining data from a randomized controlled trial of a motivational interviewing-based intervention for problem drinkers found that high levels of therapeutic bond and understanding between patient and therapist predicted decreased alcohol use at the end of treatment. This study highlights the importance of relational components in motivational interviewing treatments for alcohol use.
The quality of the relationship between a therapist and his or her client can make a significant contribution to recovery from substance use disorders. Treatments often harness aspects of therapeutic relationships (e.g., therapeutic bond) to positively affect therapeutic outcomes. Within motivational interviewing (MI), for example, authors theorize that a relational component is 1 active component that affects change. The present study aims to examine the effects of relationships within a treatment setting on drinking. A secondary data analysis was performed on data collected from problem drinkers in a randomized controlled trial. Participants were assigned to MI or relational MI without directive elements (spirit-only MI). Participants answered questions about alcohol use and therapeutic bond before, during, and at the end of an 8-week treatment period. High levels of therapeutic bond and empathic resonance predicted decreased alcohol use at the end of treatment for participants in both conditions. This study highlights the importance of relational components in treatments for substance abuse. (Wiprovnick A, Kuerbis A and Morgenstern J. Psychology of Addictive Behaviors, 29(1): 129-135.)
Significance: It has been difficult to establish a causal link between alcohol use and sexual behavior due to methodological limitations. Experimental methods are better able than other approaches to find such a link. This meta-analysis, which evaluated experimental studies on the effects of alcohol consumption on unprotected sex intentions, found that alcohol use was associated with greater intentions to engage in unprotected sex, weaker sexual communication and negotiation skills, and higher levels of sexual arousal. Addressing alcohol consumption as a key component in sexual risk-taking may lead to more effective interventions for sexual risk behavior and its potential adverse consequences, including HIV.
Alcohol is associated with HIV and other sexually transmitted infections through increased sexual risk-taking behavior. Establishing a causal link between alcohol and sexual behavior has been challenging due to methodological limitations (e.g., reliance on cross-sectional designs). Experimental methods can be used to establish causality. The purpose of this meta-analysis was to evaluate the effects of alcohol consumption on unprotected sex intentions. We searched electronic bibliographic databases for records with relevant keywords; 26 manuscripts (k = 30 studies) met inclusion criteria. Results indicate that alcohol consumption is associated with greater intentions to engage in unprotected sex (d +s = 0.24, 0.35). The effect of alcohol on unprotected sex intentions was greater when sexual arousal was heightened. Alcohol consumption is causally linked to theoretical antecedents of sexual risk behavior, consistent with the alcohol myopia model. Addressing alcohol consumption as a determinant of unprotected sex intentions may lead to more effective HIV interventions. (Scott-Sheldon LA, Carey KB, Cunningham K, Johnson BT, Carey MP; MASH Research Team. AIDS Behav. 2015 Jun 17. [Epub ahead of print])
Significance: Hepatocellular carcinoma (HCC), the most common form of liver cancer, has a high mortality rate and no adequate treatment. The most common underlying factor of HCC is cirrhosis caused by viral hepatitis, chronic alcoholism, or obesity. This study examined the involvement of the hepatic cannabinoid 1 receptors (CB1R) in HCC using liver biopsy samples from HCC patients (without viral hepatitis) and from mice with carcinogen-induced HCC. Investigators found that blockade or genetic deletion of CB1R suppresses the growth of HCC through specific mechanisms, underscoring the therapeutic potential of peripheral CB1R blockade in HCC.
Hepatocellular carcinoma (HCC) has high mortality and no adequate treatment. Endocannabinoids interact with hepatic cannabinoid 1 receptors (CB1Rs) to promote hepatocyte proliferation in liver regeneration by inducing cell cycle proteins involved in mitotic progression, including Forkhead Box M1. Because this protein is highly expressed in HCC and contributes to its genesis and progression, we analyzed the involvement of the endocannabinoid/CB1R system in murine and human HCC. Postnatal diethylnitrosamine treatment induced HCC within 8 months in wild-type mice but fewer and smaller tumors in CB1R–/– mice or in wild-type mice treated with the peripheral CB1R antagonist JD5037, as monitored in vivo by serial magnetic resonance imaging. Genome-wide transcriptome analysis revealed CB1R-dependent, tumor-induced up-regulation of the hepatic expression of CB1R, its endogenous ligand anandamide, and a number of tumor-promoting genes, including the GRB2 interactome as well as Forkhead Box M1 and its downstream target, the tryptophan-catalyzing enzyme indoleamine 2,3-dioxygenase. Increased indoleamine 2,3-dioxygenase activity and consequent induction of immunosuppressive T-regulatory cells in tumor tissue promote immune tolerance. Conclusion: The endocannabinoid/CB1R system is up-regulated in chemically induced HCC, resulting in the induction of various tumor-promoting genes, including indoleamine 2,3-dioxygenase; and attenuation of these changes by blockade or genetic ablation of CB1R suppresses the growth of HCC and highlights the therapeutic potential of peripheral CB1R blockade. (Mukhopadhyay B, Schuebel K, Mukhopadhyay P, Cinar R, Godlewski G, Xiong K, Mackie K, Lizak M, Yuan Q, Goldman D, and Kunos G. Hepatology, 2015 May;61(5):1615-26.doi:10.001/hep.27686.Epub 2015 Feb17.)
Fat-Specific Protein 27/Cidec Promotes Development of Alcoholic Steatohepatitis In Mice and Humans
Significance: Hepatic fat-specific protein 27/CIDEC expression is highly upregulated in chronic-plus-binge ethanol-fed mice and in patients with alcoholic hepatitis. Inhibition of fat-specific protein 27 ameliorates liver injury in ethanol-fed mice, and hepatic fat-specific protein 27 levels correlate with disease severity in patients. These findings suggest that fat-specific protein 27 plays an important role in promoting development of alcoholic steatohepatitis in mice and patients, thus indicating a novel pharmacologic target for treatment.
BACKGROUND & AIMS: Alcoholic steatohepatitis (ASH) is the progressive form of alcoholic liver disease and may lead to cirrhosis and hepatocellular carcinoma. We studied mouse models and human tissues to identify molecules associated with ASH progression, and focused on mouse fat-specific protein 27 (FSP-27)/human cell death-inducing DFF45-like effector C (CIDEC) protein, which is expressed in white adipose tissues and promotes formation of fat droplets. METHODS: C57BL/6N mice or mice with hepatocyte-specific disruption of Fsp27 (Fsp27Hep-/- mice) were fed the Lieber-Decarli ethanol liquid diet (5% ethanol) for 10 days to 12 weeks, followed by 1 or multiple binges of ethanol (5 or 6 g/kg) during the chronic feeding. Some mice were given an inhibitor of the peroxisome proliferator-activated receptor-γ (PPARG) (GW9662). Adenoviral vectors were used to express transgenes or small hairpin (sh) RNAs in cultured hepatocytes and in mice. Liver tissue samples were collected from ethanol-fed mice or from 31 patients with alcoholic hepatitis (AH) with biopsy-proved ASH and analyzed by histologic, immunohistochemical, transcriptome, immunoblot, and real-time PCR analyses. RESULTS: Chronic-plus-binge ethanol feeding of mice, which mimics the drinking pattern of patients with AH, produced severe ASH and mild fibrosis. Microarray analyses revealed similar alterations in expression of many hepatic genes in ethanol-fed mice and humans with ASH, including upregulation of mouse Fsp27 (also called Cidec) and human CIDEC. Fsp27Hep-/- mice and mice given injections of adenovirus-Fsp27shRNA had markedly reduced ASH following chronic-plus-binge ethanol feeding. Inhibition of PPARG and cyclic AMP-responsive element binding protein H (CREBH) prevented the increases in Fsp27α and FSP27β mRNAs, respectively, and reduced liver injury in this chronic-plus-binge ethanol feeding model. Overexpression of FSP27 and ethanol exposure had synergistic effects in inducing production of mitochondrial reactive oxygen species and damage to hepatocytes in mice. Hepatic CIDEC mRNA expression was increased in patients with AH and correlated with the degree of hepatic steatosis and disease severity including mortality. CONCLUSION: In mice, chronic-plus-binge ethanol feeding induces ASH that mimics some histological and molecular features observed in patients with AH. Hepatic expression of FSP27/CIDEC is highly upregulated in mice following chronic-plus-binge ethanol feeding and in patients with AH; this upregulation contributes to alcohol-induced liver damage (Xu MJ, Cai Y, Wang H, Altamirano J, Chang B, Bertola A, Odena G, Lu J, Tanaka N, Matsusue K, Matsubara T, Mukhopadhyay P, Kimura S, Pacher P, Gonzalez FJ, Bataller R, Gao B: Gastroenterology. 2015 Jun 19. pii: S0016-5085(15)00866-5. doi: 10.1053/j.gastro.2015.06.009. [Epub ahead of print])
Significance: A hallmark of liver fibrosis is the activation of hepatic stellate cells (HSC) which results in their production of fibrotic molecules, a process that is largely regulated by connective tissue growth factor (CCN2). This study identified transcription factor Twist1 as a product of quiescent HSC in adult mice which indirectly inhibits CCN2 production through its transcriptional activation of micro RNA-214. During HSC activation, higher levels of CCN2 result, at least in part, from decreased expression of Twist1, resulting in reduced miR-214 transcription. This study reveals a previously unrecognized role for Twist1 as a suppressor of CCN2 expression and its downstream fibrogenic signals and highlights the potential utility of Twist1, miR-214, and CCN2 as novel circulating biomarkers for liver fibrosis.
Abstract. A hallmark of liver fibrosis is the activation of hepatic stellate cells (HSC) which results in their production of fibrotic molecules, a process that is largely regulated by connective tissue growth factor (CCN2). CCN2 is increasingly expressed during HSC activation due to diminished expression of microRNA-214 (miR-214), a product of dynamin 3 opposite strand (DNM3os) that directly suppresses CCN2 mRNA. We show that an E-box in the miR-214 promoter binds the basic helix-loop-helix transcription factor, Twist1, which drives miR-214 expression and results in CCN2 suppression. Twist1 expression was suppressed in HSC of fibrotic livers or in cultured HSC undergoing activation in vitro or after treatment with ethanol. Further, Twist1 decreasingly interacted with DNM3os as HSC underwent activation in vitro. Nanovesicular exosomes secreted by quiescent but not activated HSC contained high levels of Twist1, thus reflecting the suppression of cellular Twist1 during HSC activation. Exosomal Twist1 was intercellularly shuttled between HSC and stimulated expression of miR-214 in the recipient cells, causing expression of CCN2 and its downstream effectors to be suppressed. Additionally, the miR-214 E-box in HSC was also regulated by hepatocyte-derived exosomes showing that functional transfer of exosomal Twist1 occurs between different cell types. Finally, the levels of Twist1, miR-214 or CCN2 in circulating exosomes from fibrotic mice reflected fibrosis-induced changes in the liver itself, highlighting the potential utility of these and other constituents in serum exosomes as novel circulating biomarkers for liver fibrosis. These findings reveal a novel function for cellular or exosomal Twist1 in CCN2-dependent fibrogenesis. (Chen L, Chen R, Kemper S, Charrier A, Brigstock DR. Am J Physiol Gastrointest Liver Physiol. 2015 Jul 30 [Epub ahead of print]).
Effect of Roux-en-Y Gastric Bypass Surgery on Alcohol Pharmacokinetics
Significance: Roux-en-Y gastric bypass surgery (RYGB), a common surgical intervention for weight control, is associated with an increased risk of developing AUD. In this study, women who underwent RYGB reached the same blood alcohol concentration in half the number of drinks and reported a greater feeling of drunkenness compared to women who didn’t have the surgery. RYGB-positive women also exceeded the legal driving limit for blood alcohol content 30 minutes after alcohol ingestion and met the criteria used to define an episode of binge drinking, whereas RYGP-negative women who consumed the same amount of alcohol did not. These data underscore the need to make patients aware of the alterations in alcohol metabolism that occur after RYGB surgery to help reduce the risk of potential serious consequences of moderate alcohol consumption.
Roux-en-Y gastric bypass (RYGB) is the most common bariatric surgical procedure performed in the world.1 Although RYGB surgery causes a marked reduction in food intake and induces remission of food addiction,2 it is associated with an increased risk of developing alcohol use disorders.3 It is likely that RYGB-related changes in gastrointestinal anatomy alter the pharmacokinetics and subjective effects of ingested alcohol,4 which contributes to the increased risk of alcohol use disorders. However, results from previous studies are limited because (1) blood alcohol concentrations (BACs) were measured in venous blood samples, which underestimates the peak BAC delivered to the brain in patients who have had RYGB surgery, and (2) the subjective effects of alcohol have not been assessed using validated questionnaires. The purpose of the present study was to evaluate the effect of RYGB on the pharmacokinetics and subjective effects of ingested alcohol, using arterialized blood samples and a validated questionnaire. (Pepino MY, Okunade AL, Eagon JC, Bartholow BD, Bucholz K, Klein S: JAMA Surg. 2015 Aug 5. doi: 10.1001/jamasurg.2015.1884. [Epub ahead of print])
Press and Publications Activities:
Recent News Media Interviews
Dr. Koob continues to field numerous interviews from national and international news outlets on timely topics related to NIAAA’s research and its impact on treatment and prevention of alcohol abuse and AUD. Notable interviews since June include CNN, U.S. News & World Report, Cosmopolitan magazine, Psychiatric News, and Yahoo Health.
Publication Statistics
As of July, there were 29,832 subscribers to the Alcohol Alert; 29,124 to Alcohol Research: Current Reviews; 19,017 to the NIAAA Spectrum; and 18,629 to receive general information.
Press Releases
NIH study identifies gene variant linked to compulsive drinking (July 20, 2015 – also appeared in the NIH Record)
NIH begins clinical trial of new medication for alcohol use disorder (June 25, 2015)
NIAAA honors Jonathan Gibralter with Senator Harold Hughes Award (June 10, 2015)
NIH study finds alcohol use disorder on the increase (June 3, 2015)
Study defines brain and behavioral effects of teen binge drinking (April 2, 2015)
Partnerships, Outreach & Public Liaison Activities
Partnerships
Since June, the Communications and Public Liaison Branch has initiated new collaborative projects with a number of new and existing liaison groups:
- Developed a publication distribution partnership with Guard Your Health, an organization that provides health resources and information to members of the National Guard.
- Al-Anon posted and publicized a podcast with Dr. Bob Huebner highlighting issues covered in our publications, including Rethinking Drinking and Treatment for Alcohol Problems.
- NIAAA is partnering with NIDA on National Drug and Alcohol Facts Week, a week of events geared towards educating kids and parents about the dangers of drugs and alcohol. The week will take place in January 2016.
NIAAA Social Media
The NIAAA Twitter account (@NIAAAnews) now has over 12,400 followers. In addition to the Wearable Biosensor Competition Chat, NIAAA also recently hosted a chat with NIDA on drugged/drunk driving, which focused on driving impairment after alcohol/marijuana use in combination and alone. Mr. Gregory Bloss served as NIAAA’s scientific expert.
Summer Safety Outreach
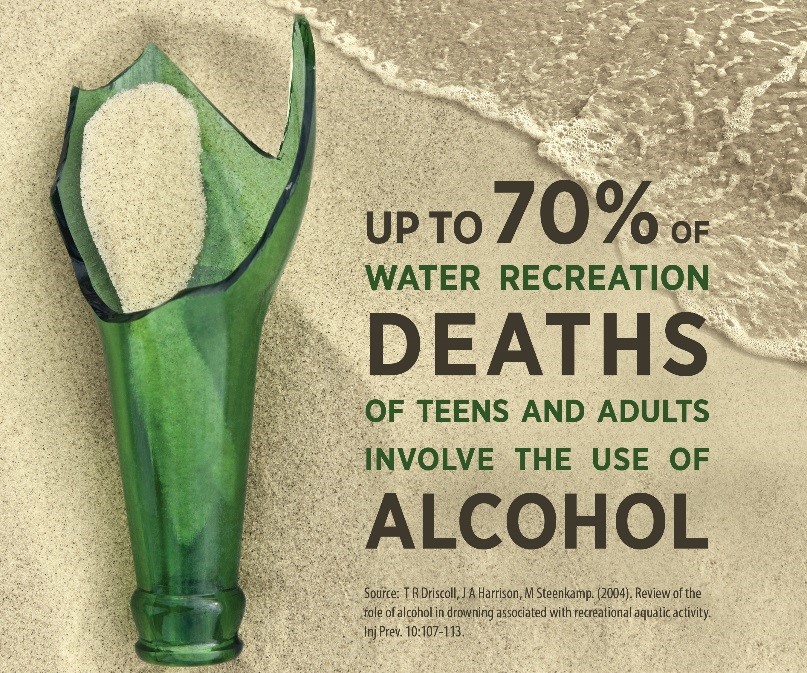 For the summer safety installment of the seasonal outreach series, NIAAA disseminated its fact sheet titled, “Risky Drinking Can Put a Chill on Your Summer Fun” to the media through PR Newswire on July 1, 2015. The fact sheet was posted by Internet news outlets such as Reuters, The Boston Globe, the Star Tribune, the Lexington Herald-Ledger, and the Sacramento Bee, as well as business journals, industry publications, and numerous local affiliates of major television networks (ABC, NBC, CBS, and Fox)nationwide. The release had a total of 200 media links, representing a total potential audience of 20,429,000 people.
For the summer safety installment of the seasonal outreach series, NIAAA disseminated its fact sheet titled, “Risky Drinking Can Put a Chill on Your Summer Fun” to the media through PR Newswire on July 1, 2015. The fact sheet was posted by Internet news outlets such as Reuters, The Boston Globe, the Star Tribune, the Lexington Herald-Ledger, and the Sacramento Bee, as well as business journals, industry publications, and numerous local affiliates of major television networks (ABC, NBC, CBS, and Fox)nationwide. The release had a total of 200 media links, representing a total potential audience of 20,429,000 people.
Fetal Alcohol Spectrum Disorder Awareness Day Activities
To recognize FASD Awareness Day, celebrated on September 9 each year, NIAAA partnered with the National Organization on Fetal Alcohol Syndrome for a chat featuring Dr. Ken Warren as NIAAA’s scientific expert. We also highlighted FASD Awareness Day with a special web carousel posted to the NIAAA site (below) and by sharing social media messages throughout the month. The day is intended to raise awareness that prenatal alcohol exposure is the leading preventable cause of birth defects and developmental disorders in the United States.

NIAAA’s Wearable Alcohol Biosensor Challenge
NIAAA continues to promote the Alcohol Biosensor Challenge through the press, social media, graphic message placements, and targeted outreach to potential applicants. We have worked to reach the biotech community, professional audiences, and academia by contacting top science and tech magazines, bloggers, biotech and biomedical engineering programs at U.S. colleges, entrepreneurial programs, and by promoting the competition at top biotech conferences. Highlights from these efforts include a full-page advertisement in Scientific American magazine (as well as a web banner and e-blast to their readers), a blog post on popular biotech blog (MedGadget), and an article on the Engineering in Medicine & Biology Society webpage (EMBS). EMBS is the world’s largest international society of biomedical engineers. MedGadget blog has about 500K unique monthly visitors. This post was also distributed via Facebook (12.5K), Twitter (25K), and LinkedIn (3K).

Biosensor Twitter Chat & Social Media Outreach
NIAAA hosted a Twitter Chat with the biosensor competition coordinators Dr. Kathy Jung and F.L. Dammann that had an estimated reach of 1.3 million accounts and 2.2 million impressions (number of times a tweet using the #AlcoholBiosensor hashtag could have been seen). During the chat, members of the public were able to have questions about the competition answered.
Eric Topol, the editor-in-chief of Medscape, noted NIAAA’s creativity in promoting the biosensor competition by tweeting that the announcement was “not your typical government ad” to his 67,000 Twitter followers.
Outreach to Academia 
A drop-in feature about the competition and related graphic was sent to department chairs for bioengineering, engineering, and biotechnology programs, as well as professors specializing in wearable tech. Entrepreneurship programs were also notified.
Promotion in Scientific American
A full-page color print ad appeared in the August issue of Scientific American. The magazine also ran a web banner ad (viewed 268,944 times during June 2015), tablet ad, and sent an email blast to its readers. Scientific American is ranked #4 in readers with a post-graduate education, and its website has 5.6M unique visitors per month.