NIAAA Director's Report on Institute Activities to the 142nd Meeting of the National Advisory Council on Alcohol Abuse and Alcoholism
Table of Contents
- NIAAA BUDGET
- LEGISLATIVE NEWS
- COLLABORATIVE RESEARCH ON ADDICTION AT NIH UPDATE
- DIRECTOR'S ACTIVITIES
- WEARABLE ALCOHOL BIOSENSOR CHALLENGE PRIZES AWARDED
- STAFF TRANSITIONS
- NEW REQUESTS FOR APPLICATIONS AND PROGRAM ANNOUNCEMENTS
- NOTABLE NIAAA STAFF ACTIVITIES
- NIAAA-LED GRANTEE TRAINING SESSIONS
- WHAT'S AHEAD
- NIH RESEARCH HIGHLIGHTS
- NIAAA COMMUNICATIONS ACTIVITIES
Fiscal Year (FY) 2016
After a lengthy continuing resolution, H.R.2029 - Consolidated Appropriations Act, 2016 was signed into law by President Obama on December 18, 2015.
The National Institutes of Health (NIH) received a total of $32 billion, $2 billion above the FY 2015 enacted level. This funding provides support for the Precision Medicine Initiative and includes specific increases for Alzheimer’s disease research, the Brain Research through Advancing Innovative Neurotechnologies (BRAIN) Initiative, antibiotic resistance research, and the Institutional Development Award program. The bill provides a general increase to all NIH Institutes and Centers, and it continues support for the Gabriella Miller Kids First Pediatric Research program (Kids First).
The FY 2016 appropriation for NIAAA provides $467.7 million. This represents a $20.5 million, or 4.9 percent, increase over the FY 2015 budget level. The NIAAA appropriation includes a $2.7 million set-aside for the BRAIN Initiative. NIAAA estimates that it will support a total of 684 research project grants (RPG) in FY 2016 compared to 668 in 2015, and 111 individual fellowships in 2016 compared to 104 in 2015.
FY 2017
On February 9, 2016, President Obama submitted to Congress the FY 2017 President’s Budget request for all federal agencies. Included in this request is a proposed budget for the NIH of $33.136 billion, $825 million more than the FY 2016 enacted level for NIH. The NIAAA budget request of $467.5 million is flat compared to the FY 2016 NIAAA enacted budget.
| Mechanism | FY2015 Actual |
FY 2016* Enacted |
FY 2017 President's Budget |
|||
|---|---|---|---|---|---|---|
| Number | Amount | Number | Amount | Number | Amount | |
| Research Projects | ||||||
| Noncompeting | 489 | $187,270 | 479 | $187,985 | 451 | $182,100 |
| Administrative Supplements | (9) | 2,091 | (13) | 2,600 | (32) | 2,600 |
| Competing | 156 | 52,828 | 173 | 58,350 | 182 | 61,494 |
| Subtotal, RPGs | 645 | 242,189 | 652 | 248,935 | 633 | 246,194 |
| SBIR/STTR | 23 | 10,449 | 32 | 11,279 | 32 | 11,960 |
| Research Project Grants | 668 | 252,638 | 684 | 260,214 | 665 | 258,154 |
| Research Centers | ||||||
| Specialized/Comprehensive | 18 | 28,019 | 20 | 30,264 | 20 | 30,021 |
| Clinical Research | - | - | - | - | - | - |
| Biotechnology | - | - | - | - | - | - |
| Comparative Medicine | - | - | - | - | - | - |
| Res. Centers in Minority Instit. | - | - | - | - | - | - |
| Subtotal, Centers | 18 | 28,019 | 20 | 30,264 | 20 | 30,021 |
| Other Research | ||||||
| Research Careers | 88 | 14,024 | 92 | 14,445 | 92 | 14,500 |
| Cancer Education | - | - | - | - | - | - |
| Cooperative Clinical Research | 1 | 7,250 | 2 | 9,466 | 2 | 9,466 |
| Biomedical Research Support | - | - | - | - | - | - |
| Minority Biomed. Research Support | - | 340 | - | 340 | - | 340 |
| Other | 46 | 15,628 | 48 | 16,097 | 48 | 16,097 |
| Subtotal, Other Research | 135 | 37,242 | 142 | 40,348 | 142 | 40,403 |
| Total Research Grants | 821 | 317,899 | 846 | 330,826 | 827 | 328,578 |
| Training | ||||||
| Individual | 104 | 4,234 | 111 | 4,580 | 111 | 4,656 |
| Institutional | 173 | 8,456 | 173 | 8,609 | 173 | 8,751 |
| Total, Training | 277 | 12,689 | 284 | 13,189 | 284 | 13,407 |
| Research & Develop. Contracts | 68 | 36,614 | 69 | 40,283 | 69 | 40,650 |
| (SBIR/STTR) | (4) | (1,100) | (4) | (1,916) | (4) | - |
| Intramural Research | 107 | 49,471 | 99 | $49,644 | 99 | $50,637 |
| Res. Management & Support | 130 |
30,478 |
138 |
$33,503 (10) |
140 |
$34,173 |
| Total, NIAAA | $447,152 | $467,445 | $467,445 | |||
*FY 2016 budget excludes the $255K AIDS transfer
In 2015, the House Energy and Commerce Committee passed the 21st Century Cures Act with the goal of enhancing and accelerating the discovery, development, and delivery of new treatments and cures. This bill designated $8.75 billion for the NIH and $550 million for the U.S. Food and Drug Administration (FDA) over a five-year period. In 2016, the Senate Health, Education, Labor and Pensions (HELP) Committee held three executive review sessions to consider provisions for a Senate counterpart to the House measure. Although the HELP Committee has drafted the legislation, funding levels for the NIH and FDA have not been determined. Once an agreement on funding has been reached, it is hoped that the draft bill will move forward for consideration by the full Senate.
COLLABORATIVE RESEARCH ON ADDICTION AT NIH UPDATE
Adolescent Brain and Cognitive Development (ABCD) Study
The ABCD study is making progress towards meeting its goal of beginning subject recruitment in fall 2016. Currently, protocols for both the imaging portion of the study and the neuropsychological portions are being pilot tested and finalized. More extensive pilot testing will take place over the summer. Centralized institutional review board (IRB) approval has been received. Study recruitment efforts have been given a boost by official endorsements from the American Association of School Superintendents, the American School Health Association, and a number of state school districts. The study website continues to be updated with sections for scientists, educators, and parents and can be seen at http://abcdstudy.org/.
In addition, a flyer to aid in recruitment can be downloaded at https://www.drugabuse.gov/sites/default/files/nida_abcdflyer.pdf.
New Collaborative Research on Addiction at NIH (CRAN) Notice of Funding Opportunities (NOFOs)
The CRAN Steering Committee has approved new NOFOs that will focus on multi-substance research. The first initiative, Integrative Research on Polysubstance Abuse and Addiction, is focused on translational studies that aim to (1) characterize how the neurobiological alterations, associated behaviors, and public health consequences arising from polysubstance use differ from, or are similar to, those observed in single drug use; and (2) promote integrative polysubstance research along a translational pipeline, consisting of basic science research in animals, human-based laboratory investigations, and epidemiological studies.
These dual objectives will be accomplished with a Phased Innovation (R21/R33) mechanism, where polysubstance research can occur in any of these translational stages during the R21 phase and these findings will be rapidly back- or forward-integrated into another stage during the R33 phase, allowing for bi-directional research exchange.
The second initiative, Target Assessment, Engagement and Data Replicability to Improve Substance Use Disorder Treatment Outcomes, consists of two program announcements (PAs) focused on treatment development:
-
- Studies that focus on early-stage treatment generation and pilot clinical trials that are consistent with an experimental therapeutic approach. This NOFO provides support for up to two years (Phase I; R21) for protocol development, target identification, and studies to confirm target engagement (i.e., link targets with tangible outcomes); followed by up to 3 years of support (Phase II; R33) for replication studies of addiction treatment across 2 or more settings.
- Studies of novel treatments that include behavioral, pharmacological, physiological, learning- and device-based treatment approaches and targets thereof. The purpose of this NOFO is to provide support for applications that focus on data replication and the scalability of novel, targeted addiction treatments. Studies of novel treatments include, but are not limited to: behavioral, pharmacological, biologics-based, cognitive, device-based, interpersonal, physiological, or combined approaches. The R33 (Phase II) funding mechanism provides support for up to 3 years for replication studies of addiction treatment across 2 or more settings.
A meeting of investigators who received awards under the CRAN request for applications (RFA), “Using Social Media to Understand and Address Substance Use and Addiction,” will take place on June 22, 2016, in Rockville, Maryland.
Additional information on all CRAN activities and studies can be found at http://addictionresearch.nih.gov.
NIAAA’s Director, Dr. George F. Koob, made a number of important presentations between January and May 2016.
- He was invited to present one of the seminars in the Dean Biomedical Seminar Series, a major seminar series at Virginia Commonwealth University School of Medicine, Richmond, Virginia, on March 9, 2016. His presentation was titled, “Neuroplasticity in the Brain Stress Systems in Addiction.”
- He delivered the 24th Annual Albert Barrett Neuroscience Lecture at the University of Michigan in Ann Arbor, Michigan, on March 30, 2016. The title of the lecture was “Neurobiology of Addiction: A Stress Surfeit Disorder.”
- He was an invited speaker at this year’s annual Addiction Symposium at Pennsylvania State University College of Medicine in Hershey, Pennsylvania, on April 4, 2016. The subject of his talk was “Neuroplasticity in the Brain Stress Systems in Addiction.”
- He was invited to give a lecture at the Center for Clinical and Cognitive Neuroscience, San Diego State University, San Diego, California, on April 22, 2016. The title of his lecture was “Neurobiology of Addiction: A Stress Surfeit Disorder.”
- He was a featured speaker at a May 5, 2016, congressional briefing titled, “Alcohol, Stress, and the Brain: Implications for Treatment and Recovery”. The briefing was sponsored by the Friends of NIAAA in cooperation with the Congressional Addiction, Treatment, and Recovery Caucus, and the Military Mental Health Caucus.
- He was a plenary speaker at the International Society Developmental Neuroscience 2016 in Juan-les-Pins, Antibes, France, on May 14, 2016. The title of his talk was “Addiction as a Stress Surfeit Disorder.”
- He was the keynote speaker at the Sixth Annual Aspen.
WEARABLE ALCOHOL BIOSENSOR CHALLENGE PRIZES AWARDED

In May 2016, NIAAA announced the winners of its Wearable Alcohol Biosensor Challenge, a competition to design a discreet device capable of measuring blood alcohol levels in near real-time. The winning prototype and recipient of the $200,000 first prize was submitted by BACtrack, a company known nationally for designing and selling portable breath alcohol testers for consumer use. Their entry, the BACtrack Skyn, is worn on the wrist and offers continuous and non-invasive monitoring of a user’s blood alcohol content (BAC). NIAAA publicized the prize by issuing a press release with an accompanying video and robust social media outreach, resulting in national attention for the competition. Articles about the winners appeared in the Journal of the American Medical Association, Reuters, Popular Science, The Telegraph, Yahoo News, Voice of America, Engadget, IEEE Spectrum, and others.

Kim Bochniak recently joined the NIAAA Administrative Services Branch in the role of Inventory Management Specialist. Previously, she was with the NIAAA Division of Intramural Clinical and Biological Research. In her new position, Ms. Bochniak is responsible for the day-to-day custody, use, care, and safekeeping of all NIAAA property in both the intramural and extramural programs.

Christie Halcomb recently joined the NIAAA Administrative Services Branch as Program Specialist supporting NIAAA’s Extramural and Intramural Programs, and the Office of the Director. Christie comes to NIAAA from the National Cancer Institute (NCI), where she served as a Program Analyst. Previously, she was a Lead Purchasing Agent at the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).

Celia Burke Herlihy joined the Grants Management Branch/Office of Extramural Activities (OEA), on May 14, 2016, as a Grants Management Specialist. Ms. Herlihy comes to NIAAA from the National Institute of Allergy and Infectious Diseases, where she had served as a Grants Management Specialist since 2012 and was responsible for a grant portfolio that included the most complex grant mechanisms. Prior to joining NIH, she was a legal assistant at the Social Security Administration.

Desiree Marshall-Brown transferred to the Department of Homeland Security. Ms. Marshall-Brown worked in NIAAA for three years as a Staff Assistant to the Executive Officer in the Office of Resource Management.
Katrina Foster, Scientific Review Officer in the Extramural Project Review Branch/OEA, left NIAAA on April 16, 2016, to join the administrative staff at the Veterans Health Administration, Washington, D.C.
NEW REQUESTS FOR APPLICATIONS (RFAs) AND PROGRAM ANNOUNCEMENTS (PAs)
Issued by NIAAA
Targets of Low-Dose Alcohol in the Brain (R01, R21) (RFA-AA-16-008, RFA-AA-16-009): This NOFO solicits research grant applications that define molecular and cellular targets mediating alcohol effects at concentrations of 10 mM and below. It has been well established that alcohol at relatively high concentrations modulates a variety of receptors and ion channels, intracellular signaling cascades, and gene expression in the brain. Significant knowledge gaps, however, remain in understanding how the brain responds to low doses of alcohol and what molecular targets mediate alcohol action at concentrations below 10 mM. The purpose of this NOFO is to support research efforts to identify targets mediating effects of low-dose alcohol at molecular, cellular, and circuit levels.
Program for Extramural/Intramural Alcohol Research Collaborations (U01) (PAR-16-214): The purpose of this NOFO is to encourage collaboration between alcohol researchers in the extramural community and those within the NIAAA intramural research program. The objective of this NOFO is to bring together the research expertise that, as a functioning collaborative unit, will address key alcohol-based research questions that would not otherwise be possible by the same individuals working towards similar goals in isolation. The NIH Intramural Scientist will be a tenured or tenure-track scientist from the NIAAA Intramural Research Program, with whom the Project Director/Principal Investigator has made prior contact for the collaborative project.
Specialized Alcohol Research Centers (P50) (RFA-AA-17-001): The overall purpose of the NIAAA Alcohol Research Center program is to provide leadership in conducting and fostering interdisciplinary, collaborative research on a wide variety of topics relevant to the Institute’s mission. These topics include, but are not limited to: the nature, etiology, genetics, diagnosis, treatment, and prevention of alcohol use disorders (AUDs) and their biomedical, psychosocial, and economic consequences across the lifespan. Centers also are regional or national resources that contribute to the development of new research methods, technologies and approaches that sustain innovative goal-directed research.
Comprehensive Alcohol Research Centers (P60) (RFA-AA-17-002): The purpose of the NIAAA Alcohol Research Center program is to provide leadership in conducting and fostering interdisciplinary, collaborative research on a wide variety of topics relevant to the Institute’s mission, and the dissemination of information to initiate and expand community education related to the activities of the center.
Limited Competition for the Continuation of the National Consortium on Alcohol and Neurodevelopment in Adolescence (NCANDA): This Notice of Funding Opportunity (NOFO) is a limited competition to support the continuation of the Research Project Sites of the National Consortium on Alcohol and Neurodevelopment in Adolescence (NCANDA). The NCANDA Research Project Sites have responsibility for the acquisition of data according to the standard protocol for the nation-wide consortium to study the impact of alcohol drinking on brain structure and function during adolescence and into early adulthood. RFA-AA-17-004 (U24) will support continuation of the NCANDA Administrative Resource, RFA-AA-17-005 will support the continuation of the NCANDA Data Analysis Resource, and RFA-AA-17-003 will support the continuation of the Research Projects Sites within the consortium.
NIH-Wide with NIAAA Participation
BD2K Mentored Career Development Award in Biomedical Big Data Science for Intramural Investigators (K22) (RFA-ES-16-003) and for Clinicians and Doctorally Prepared Scientists (K01) (RFA-ES-16-002): The first of these NOFOs issued by the National Institute of Environmental Health Sciences solicits K22 applications for an NIH Career Transition Award to provide support for outstanding basic or clinical investigators in the NIH Intramural Program to transition to independent, faculty-level academic positions in the area of Big Data Science. The initiative is a 2-phase program which includes a mentored 1-year phase in an intramural appointment at NIH, and a second phase of up to 3 years of support at an extramural institution. The second of these BD2K NOFOs solicits applications for a mentored career development award (K01) in the area of Big Data Science. The aim of this initiative is to support additional training of scientists who will gain the knowledge and skills necessary to be independent researchers as well as to work in a team environment to develop new Big Data technologies, methods, and tools applicable to basic and clinical research.
Health Services Research on Minority Health and Health Disparities (R01, R21) (PAR-16-221, PAR-16-222): The purpose of this NOFO issued by the National Institute on Minority Health and Health Disparities is to encourage innovative health services research that can directly and demonstrably contribute to the improvement of minority health and/or the reduction of health disparities at the health care system level as well as within clinical settings.
Diet and Physical Activity Assessment Methodology (R01) (PA-16-167): This NOFO issued by the National Institute of Diabetes and Digestive and Kidney Diseases encourages innovative research to enhance the quality of measurements of dietary intake and physical activity. Applications submitted under this NOFO are encouraged to include development of: novel assessment approaches; better methods to evaluate instruments; assessment tools for culturally diverse populations or various age groups, including children and older adults; improved technology or applications of existing technology; statistical methods/modeling to improve assessment and/or to correct for measurement errors or biases; methods to investigate the multidimensionality of diet and physical activity behavior through pattern analysis; or integrated measurement of diet and physical activity along with the environmental context of such behaviors.
Population Health Interventions: Integrating Individual and Group Level Evidence (R01, R21) (PA-16-146, PA-16-147): This NOFO issued by the NIH Office of Behavioral and Social Sciences Research (OBSSR) solicits applications that will improve health and reduce the burden of disease, scientific research needs to be implemented at the population level in addition to the biological and clinical levels. The purpose of this NOFO is to support multilevel, transdisciplinary population health interventions that target underlying social, economic, and environmental conditions in an effort to improve health outcomes.
Bioengineering Research Partnerships (U01) (PAR-16-116): This NOFO issued by National Institute of Biomedical Imaging and Bioengineering encourages bioengineering applications that will accelerate the development and adoption of promising tools and technologies that can address important biomedical problems. The objectives are to establish these tools and technologies as robust, well-characterized solutions that fulfill an unmet need and are capable of enhancing our understanding of life science processes or the practice of medicine. Awards will focus on supporting multidisciplinary teams that apply an integrative, quantitative bioengineering approach to developing technologies, and engage biomedical researchers or clinicians throughout the project. The goal of the program is to support projects that can realize meaningful solutions within 5–10 years.
Discovery of the Genetic Basis of Childhood Cancers and of Structural Birth Defects: Gabriella Miller Kids First Pediatric Research Program (X01) (PAR-16-150): This NOFO is an NIH Common Fund initiative inviting applications to use whole-genome sequencing to investigate the genetic etiology of structural birth defects and childhood cancers).
NOTABLE NIAAA STAFF ACTIVITIES -- FEBRUARY 2016 - MAY 2016
Dr. Veronica A. Alvarez was invited to write a commentary in the journal of Proceedings of National Academy of Science titled, “Clues on the coding of reward cues by the nucleus accumbens” The commentary was published in March 2016. (Alvarez VA. Proc Natl Acad Sci. 2016 Mar 8; 113(10):2560-2.)
Dr. Judy Arroyo served as scientific review editor and Dr. Jennifer Hobin served as editor in chief of the “Alcohol Use in Special Populations” issue of NIAAA’s journal, Alcohol Research: Current Reviews, which was released in May 2016.
Dr. Lori Ducharme co-led a workshop on implementation research for clinicians and community-based public health agencies at the National Oral Health Conference in Cincinnati, Ohio, on April 20, 2016.
Dr. Bob Freeman organized a workshop titled, “NIAAA Workshop on Emerging Trends in Underage, College, and Emerging Adult Drinking and Related Consequences,” which was held at NIAAA on May 16, 2016.
Drs. Ivana Grakalic, Soundar Regunathan, and Diana Urbanas, and Ms. Jessica Ryan presented at the 17th annual Brain Awareness Week hosted by NIH and the National Museum of Health and Medicine at Walter Reed Army Medical Center, on March 16, 2016. Various NIH Institutes with neuroscience-related programs presented hands-on demonstrations and exhibits at this event dedicated to advancing education about the brain.
Dr. Ralph Hingson presented a talk titled, “New Research since the Surgeon General’s Call to Action to Prevent and Reduce Underage Drinking” at the Community Anti-Drug Coalitions of America’s (CADCA) National Leadership Forum in National Harbor, Maryland, on February 2, 2016.
Dr. Ralph Hingson presented a talk titled, “NIAAA Research Priorities: Preventing Drug-Impaired Driving and Overdoses: Lessons from Alcohol-Impaired Driving” at the Meeting on Alcohol, Drugs, and Driving at the Pan American Health Organization in Washington, D.C., on May 5, 2016.
Dr. Robert Huebner chaired a symposium titled, “Contributions of Cognitive Neuroscience to the Treatment of Alcohol Related Problems” at the annual meeting of the Association for Psychological Science in Chicago, Illinois, on May 26, 2016.
Dr. Raye Litten presented “A Vision for the Next Decade: Medications Development to Treat Alcohol Use Disorder” in March 2016 as part of a seminar series at the Center for Studies of Addiction at the Perelman School of Medicine, University of Pennsylvania, Philadelphia, Pennsylvania.
Dr. Raye Litten organized and chaired a session titled, “Genetics of Alcohol Use Disorder” at the ASAM Annual Conference in Baltimore, Maryland, on April 17, 2016.
Dr. Raye Litten organized and chaired a panel session “Public-Private Partnerships to Develop Medications for Alcohol Use Disorder: Recent Successes and New Opportunities for Collaboration with NIAAA” at the American Society of Clinical Psychopharmacology (ASCP) meeting in Phoenix, Arizona, on May 31, 2016. In that session, he presented “New Infrastructure for Translating New Medications to Treat Alcohol Use Disorder” and “Double-Blind, Placebo-Controlled Trial Assessing the Efficacy of ABT-436 for Alcohol Dependence,” Also, Dr. Daniel Falk presented “Double-Blind, Placebo-Controlled Trial Assessing the Efficacy of Varenicline Tartrate for Alcohol Dependence.” In another panel session “Drinking Change, Consequences, and Biomarkers in Alcohol Clinical Trials: Results from the Alcohol Clinical Trials Initiative (ACTIVE),” Dr. Falk presented “World Health Organization (WHO) Risk-Level Shift Endpoints: Treatment Effects in alcohol Clinical Trials” and Dr. Litten served as a discussant.
Dr. John Matochik gave the introductory remarks at the Science of Change Conference in Atlanta, Georgia, on May 11, 2016. The theme this year was “Neuroimaging Mechanisms of Behavior Change.”
Drs. Peggy Murray, Mike Hilton and David Goldman participated with staff from four other NIH Institutes (the National Institute on Drug Abuse (NIDA), National Institute of Mental Health, National Institute on Neurological Diseases and Stroke, and the National Center for Complementary and Integrative Health) to convene Cannabinoids: A Neuroscience Research Summit March 22–23, 2016, at the Natcher Conference Center on the NIH campus, Bethesda, Maryland. Dr. Murray presented an overview of areas where NIAAA’s research priorities intersect with the marijuana research agenda including combined effects of alcohol and marijuana on fetal development, effects on adolescent development, drinking and drugged driving, epidemiology of use and disorders, and increasing our understanding of addiction; Dr. Hilton co-chaired a session on policy research; and Dr. Goldman co-chaired a session with Dr. Wilson Compton, NIDA, on alcohol, mental illness, and marijuana titled, “Psychosis, Addiction and Alcohol Interactions.”
Dr. Pal Pacher was an invited speaker in a symposium on “Novel Targets for Treatment of Cardiometabolic Diseases” at the American Society for Pharmacology and Experimental Therapeutics Annual Meeting at Experimental Biology 2016, in San Diego, California, April 2–6, 2016.
Dr. Svetlana Radaeva, in her role as project scientist on NIAAA’s alcoholic hepatitis consortia, was invited to co-chair a session titled “Interactions of the Liver with Other Organs (Gut-Liver-Brain-Adipose Axis)” at the Emerging Trends in Alcoholic Hepatitis Meeting in Miami, Florida, on January 22–23, 2016.
Dr. Deidra Roach chaired a symposium on screening, brief intervention, and referral to treatment (SBIRT) for women and girls at the American Society of Addiction Medicine (ASAM) Annual Conference on April 15, 2016. This was the second in a series of symposia sponsored by NIAAA to promote the adoption of routine SBIRT for women and girls in primary care and specialty health care settings.
Dr. Marcia S. Scott organized and presented in a symposium titled, “Case Ascertainment for Fetal Alcohol Spectrum Disorders: Implications for Screening and Preventive Intervention in Diverse Populations” at the Society for Prevention Research in San Francisco, California, on June 3, 2016.
NIAAA-LED GRANTEE TRAINING SESSIONS
Dr. Anita Bechtholt led a workshop for young and new investigators titled, “A Look Inside the Funding Process at NIAAA” during the Collaborative Perspectives on Addiction meeting in San Diego, California, on March 18, 2016.
Dr. John Matochik participated in the “NIH Panel Session: Demystifying NIH for the Early Career Investigator” at the Society of Biological Psychiatry annual meeting in Atlanta, Georgia, on May 13, 2016.
Dr. Peggy Murray gave a presentation titled, “Setting Priorities in Alcohol Research and Writing a Successful Research Proposal” at the Alcohol Research Training conference held in Kiev, Ukraine, in February 2016.
Dr. Marcia S. Scott was an invited speaker in a seminar titled, “NIH Grantspersonship: Opportunities to Fund Research and Training” at the Society for Behavioral Medicine on March 30, 2016. She gave a presentation on “NIAAA Research Priorities.” The 6-hour seminar was organized by the NIH OBSSR to provide participants information and advice on writing competitive applications for NIH funding.
The NIAAA Clinical Investigations Group’s (NCIG) multi-site clinical trial of gabapentin enacarbil has reached the 75 percent recruitment milestone. The plan is to recruit a total of 348 subjects by spring 2017. This trial is conducted through a partnership between NIAAA and XenoPort Inc.
A grantee meeting of the CRAN “Social Media” Research Consortium will be held at NIAAA on June 22–23, 2016. The Consortium comprises the group of grantees who were funded by NIAAA, NIDA, and the National Cancer Institute under the CRAN RFA-CA-14-008 (“Using Social Media to Understand and Address Substance Use and Addiction”). Dr. Robert Freeman represents NIAAA on the Consortium steering committee. All are welcome to attend.
At the Annual Scientific Meeting of the Research Society on Alcoholism (RSA) in New Orleans, Louisiana, NIAAA Director Dr. George F. Koob will present the NIAAA Update on June 26, at 8:10 a.m. Also at RSA, NIAAA staff are organizers, moderators, or presenters in more than 35 symposia, in 3 satellite meetings, and in a number of grantsmanship training activities. For the full program and latest schedule updates, please consult the RSA website at http://www.rsoa.org/.
NIAAA and NIDA will again sponsor the Frontiers in Addiction Research Mini-Convention as a satellite meeting to the Society for Neuroscience annual meeting in San Diego, California. The mini-convention will be on November 11, 2016. The theme this year is “Relapse and Recovery: From Mechanistic Understanding to Translational Research.” Drs. John Matochik and Changhai Cui are the program contacts.
NIAAA RESEARCH HIGHLIGHTS (FEBRUARY 2016 - MAY 2016)
Significance: Alcoholic cardiomyopathy in humans develops in response to chronic excessive alcohol consumption, however good models of alcohol-induced cardiomyopathy in mice are lacking. The authors describe novel mouse models of cardiomyopathies induced by chronic plus single or multiple ethanol binges (NIAAA models). They demonstrate that even a single binge can dramatically amplify the deleterious effects of alcohol in the cardiovascular system, resulting in steatosis and in mitochondrial and cardiovascular dysfunction.
Alcoholic cardiomyopathy in humans develops in response to chronic excessive alcohol consumption, however good models of alcohol-induced cardiomyopathy in mice are lacking. Herein we describe mouse models of alcoholic cardiomyopathies induced by chronic and binge ethanol (EtOH)-feeding and characterize detailed hemodynamic alterations, mitochondrial function and redox signaling in these models. Mice were fed a liquid diet containing 5% EtOH for 10, 20, 40 days (d) combined with single/ or multiple EtOH-binges (5g/kg BW). Isocalorically pair-fed mice served as controls. Left ventricular (LV) function and morphology were assessed by invasive pressure-volume conductance approach and by echocardiography. Mitochondrial complex (I, II, IV) activities, 3-nitrotyrosine (3-NT) levels, gene expression of markers of oxidative stress (gp91phox, p47phox), mitochondrial biogenesis (PGC1α, PPARα), and fibrosis were examined. Cardiac steatosis and fibrosis were investigated by histological/immunohistochemical methods. Chronic and binge EtOH-feeding (already in 10 days EtOH plus single binge group) was characterized by contractile dysfunction (decreased slope of end-systolic pressure-volume relationship and preload recruitable stroke work), impaired relaxation (decreased time constant of LV pressure decay and dP/dtmin) and vascular dysfunction (impaired arterial elastance and lower total peripheral resistance). This was accompanied by enhanced myocardial oxidative/nitrative stress (3-NT, gp91phox, p47phox, AGTR1a) and deterioration of mitochondrial complex I, II, IV activities and mitochondrial biogenesis, excessive cardiac steatosis and higher mortality. Collectively, chronic plus binge EtOH-feeding in mice leads to alcohol-induced cardiomyopathies (NIAAA models) characterized by increased myocardial oxidative/nitrative stress, impaired mitochondrial function and biogenesis, and enhanced cardiac steatosis. (Mátyás C, Varga ZV, Mukhopadhyay P, Paloczi J, Lajtos T, Erdelyi K, Nemeth BT, Nan M, Hasko G, Gao B, Pacher P Am J Physiol Heart Circ Physiol. 2016 Apr 22:ajpheart.00214.2016. doi: 10.1152/ajpheart.00214.2016. [Epub ahead of print])
Significance: Studies have found that alcohol consumption increases bacterial-derived products, specifically lipopolysaccharide (LPS) and bacterial DNA, in the portal and systemic circulation. Significantly increased levels of LPS have been found in patients with alcoholic liver disease (ALD) and in experimental animal models of ALD. The current study showed that when compared with an unsaturated fat (USF) diet, a diet rich in saturated fat (SF) prevented ethanol-induced changes in the gut microbiota and associated liver injury. Mice fed USF and ethanol developed profound liver steatosis and injury, whereas mice fed SF and ethanol were protected against ALD. The results from this study indicate that the ethanol-mediated gut dysbiosis can be therapeutically targeted by dietary manipulations that may offer a novel prevention and therapeutic approach to ALD management.
Alcoholic liver disease (ALD) ranks among major causes of morbidity and mortality. Diet and crosstalk between the gut and liver are important determinants of ALD. We evaluated the effects of different types of dietary fat and ethanol on the gut microbiota composition and metabolic activity and the effect of these changes on liver injury in ALD. Compared with ethanol and a saturated fat diet (medium chain triglycerides enriched), an unsaturated fat diet (corn oil enriched) exacerbated ethanol-induced endotoxemia, liver steatosis, and injury. Major alterations in gut microbiota, including a reduction in Bacteroidetes and an increase in Proteobacteria and Actinobacteria, were seen in animals fed an unsaturated fat diet and ethanol but not a saturated fat diet and ethanol. Compared with a saturated fat diet and ethanol, an unsaturated fat diet and ethanol caused major fecal metabolomic changes. Moreover, a decrease in certain fecal amino acids was noted in both alcohol-fed groups. These data support an important role of dietary lipids in ALD pathogenesis and provide insight into mechanisms of ALD development. A diet enriched in unsaturated fats enhanced alcohol-induced liver injury and caused major fecal metagenomic and metabolomic changes that may play an etiologic role in observed liver injury. Dietary lipids can potentially serve as inexpensive interventions for the prevention and treatment of ALD. (Kirpich IA, Petrosino J, Ajami N, Feng W, Wang Y, Liu Y, Beier JI, Barve SS, Yin X, Wei X, Zhang X, McClain CJ Am J Pathol. 2016;186(4):765-76.)
Alcohol produces distinct hepatic lipidome and eicosanoid signature in lean and obese
Significance: While clinical data indicate that obese individuals who consume alcohol are more likely to develop fatty liver disease, there is a paucity of literature on how these risk factors interact to contribute to disease pathogenesis. This study identified four principal effects of alcohol consumption on fatty liver disease: (1) an increase in cholesterol esters and diacylglycerols, (2) an increase in several hepatic phospholipids in lean mice but a depletion of phosphatidylcholine in obesity, (3) an increase in lyso-phospholipids mainly in lean mice, and (4) an increase in pro-inflammatory COX, LOX, and oxidative stress-related eicosanoids (HODEs and 11-HETE). This study provides novel insights on the complex effects of alcohol on the hepatic lipidome and the differential effects in lean versus obese state, and confirms the diversity of the effects of alcohol consumption on hepatic lipid metabolism in the background of obesity. The data also permit specific hypotheses regarding specific metabolites that can be tested in more focused mechanistic studies.
BACKGROUND AND AIMS: Alcohol and obesity related liver disease often coexists. The hepatic lipidomics due to alcohol and obesity interaction is unknown. We characterized the hepatic lipidome due to (1) alcohol consumption in lean and obese mice, and (2) obesity and alcohol interactions. METHODS: In the French-Tsukamoto mouse model, intra-gastric alcohol or isocaloric dextrose were fed with either chow (lean) or high fat high cholesterol diet (obese). Four groups - lean, lean alcohol, obese and obese alcohol were studied. Mass spectrometry was performed for hepatic lipidomics and data were analyzed. RESULTS: Alcohol significantly increased hepatic cholesterol esters and diacylglycerol in lean and obese, but was more pronounced in obese. Alcohol produced contrasting changes in hepatic phospholipids with significant enrichment in lean mice vs. significant decrease in obese mice, except phosphatidylglycerol, which was increased in both lean and obese alcohol groups. Most lysophospholipids were increased in lean alcohol and obese mice without alcohol use only. Prostaglandin-E2, 5-, 8-, and 11- hydroxyeicosatetraenoic acids, 9- and 13-hydroxyoctadecadienoic acids were considerably increased in obese mice with alcohol use. CONCLUSIONS: Alcohol consumption produced distinct changes in lean and obese with profound effects of obesity and alcohol interaction on pro-inflammatory and oxidative stress-related eicosanoids. (Puri P, Xu J, Vihervaara T, Katainen R, Ekroos K, Daita K, Min HK, Joyce A, Mirshahi F, Tsukamoto H, Sanyal AJ. J Lipid Res. 2016 Mar 28. pii: jlr.M066175. [Epub ahead of print])
Significance: These recommendations from the NIAAA Alcoholic Hepatitis (AH) consortia outline a framework for clinical research in AH as a first step toward data standardization for all variables commonly used in translational, clinical, and observational studies. The aim of these consensus recommendations is to facilitate data sharing and comparisons across studies, increasing the efficiency and effectiveness of AH research.
Heavy drinkers are at risk for a spectrum of histologic alcohol-related liver injury: steatosis, alcoholic steatohepatitis (ASH), alcohol-related fibrosis, and cirrhosis. Alcoholic hepatitis (AH), the clinical entity associated with severe ASH, has high short-term mortality. The standard-of-care therapy, prednisolone, has limited efficacy and many side effects; no other treatment has consistently shown survival benefit. The National Institute on Alcohol Abuse and Alcoholism (NIAAA)-funded Alcoholic Hepatitis Consortia carry out translational research on pathophysiologic mechanisms, genetic and environmental risk factors, phase II clinical trials, and development of biomarkers. The consortia members were convened by the National Institutes of Health to address diagnostic criteria and practical issues related to clinical AH research, and to develop a set of common data elements to harmonize ongoing and future trials. This was accomplished through 3 face-to-face meetings of the investigators and representatives of the National Institutes of Health, and subsequent electronic communications over the course of 6 months. Evidence for the recommendations was based on published trials and observational data from several of the consortia members. A draft manuscript was iteratively reviewed by members of the consortia. The goal was to reach agreements on recommendations and definitions that could facilitate trial design, and simultaneously be tested by research groups pooling their data. The recommendations made here are specifically directed to achieve better uniformity in clinical trials, rather than serving as clinical practice guidelines. (Crabb DW, Bataller R, Chalasani NP, Kamath PS, Lucey M, Mathurin P, McClain C, McCullough A, Mitchell MC, Morgan TR, Nagy L, Radaeva S, Sanyal A, Shah V, Szabo G; NIAAA Alcoholic Hepatitis Consortia. Gastroenterology. 2016;150(4):785-90.)
Significance: HIV infection is associated with elevated interleukin (IL)-6, soluble CD14, and D-dimer, which are in turn associated with mortality. Baseline measures of these biomarkers partially mediate excess mortality risk among HIV-positive versus uninfected people. Measuring inflammatory responses for alcohol users is critical for understanding HIV disease progression and mortality.
HIV infection and biomarkers of inflammation (measured by interleukin-6 [IL-6]), monocyte activation (soluble CD14 [sCD14]), and coagulation (D-dimer) are associated with morbidity and mortality. This study hypothesized that these immunologic processes mediate (explain) some of the excess risk of mortality among HIV infected (HIV+) versus uninfected people independently of co-morbid diseases. Among 2350 (1521 HIV+) participants from the Veterans Aging Cohort Study Biomarker Cohort (VACS BC) we investigated whether the association between HIV and mortality was altered by adjustment for IL-6, sCD14 and D-dimer, accounting for confounders. Participants were followed from date of blood draw for biomarker assays (baseline) until death or 7/25/2013. Analyses included ordered logistic regression and Cox Proportional Hazards regression. During 6·9 years (median), 414 deaths occurred. The proportional odds of being in a higher quartile of IL-6, sCD14 or D-dimer was 2-3 fold higher for viremic HIV+ versus uninfected people. Mortality rates were higher among HIV+ compared to uninfected people (incidence rate ratio (95% CI): 1·31 (1·06-1·62). Mortality risk increased with increasing quartiles of IL-6, sCD14 and D-dimer regardless of HIV status. Adjustment for IL-6, sCD14 and D-dimer partially attenuated mortality risk among HIV+ people with unsuppressed viremia (HIV-1 RNA≥10000 copies/mL) compared to uninfected people - hazard ratio (95% CI) decreased from 2·18 (1·60-2·99) to 2·00 (1·45-2·76). (So-Armah KA, Tate JP, Chang CH, Butt AA, Gerschenson M, Gibert CL, Leaf D, Rimland D, Rodriguez-Barradas MC, Budoff MJ, Samet JH, Kuller LH, Deeks SG, Crothers KA, Tracy RP, Crane HM, Sajadi MM, Tindle HA, Justice AC, Freiberg MS; The VACS Project Team. J Acquir Immune Defic Syndr. 2016 Feb 13.)
Risk of mortality and physiologic injury evident with lower alcohol exposureamong HIV infected compared with uninfected men
Significance: Despite antiretroviral therapy, HIV-positive men consuming more than 30 drinks per month are at increased risk of all-cause mortality and physiologic frailty. These data provide support for a recommended drinking limit for HIV-positive individuals of no more than one alcoholic drink per day, which is lower than the current levels recommended by NIAAA for men.
Background: HIV infected (HIV+) individuals may be more susceptible to alcohol-related harm than uninfected individuals. Methods: We analyzed data on HIV+ and uninfected individuals in the Veterans Aging Cohort Study (VACS) with an Alcohol Use Disorders Identification Test-Consumption AUDIT-C score from 2008 to 2012. We used Cox proportional hazards models to examine the association between alcohol exposure and mortality through July, 2014; and linear regression models to assess the association between alcohol exposure and physiologic injury based on VACS Index Scores. Models were adjusted for age, race/ethnicity, smoking, and hepatitis C infection. Results: The sample included 18,145 HIV+ and 42,228 uninfected individuals. Among HIV+ individuals, 76% had undetectable HIV-1 RNA (<500 copies/ml). The threshold for an association of alcohol use with mortality and physiologic injury differed by HIV status. Among HIV+ individuals, AUDIT-C score ≥4 (hazard ratio [HR] 1.25, 95% CI 1.09–1.44) and ≥30 drinks per month (HR, 1.30, 95% CI 1.14–1.50) were associated with increased risk of mortality. Among uninfected individuals, AUDIT-C score ≥5 (HR, 1.19, 95% CI 1.07–1.32) and ≥70 drinks per month (HR 1.13, 95% CI 1.00–1.28) were associated with increased risk. Similarly, AUDIT-C threshold scores of 5–7 were associated with physiologic injury among HIV+ individuals (beta 0.47, 95% CI 0.22, 0.73) and a score of 8 or more was associated with injury in uninfected (beta 0.29, 95% CI 0.16, 0.42) individuals. Conclusions: Despite antiretroviral therapy, HIV+ individuals experienced increased mortality and physiologic injury at lower levels of alcohol use compared with uninfected individuals. Alcohol consumption limits should be lower among HIV+ individuals. (Justice AC, McGinnis KA, Tate JP, Braithwaite RS, Bryant KJ, Cook RL, Edelman EJ, Fiellin LE, Freiberg MS, Gordon AJ, Kraemer KL, Marshall BDL, Williams EC, Fiellin DA. Drug Alcohol Depend. 1 April 2016. Doi: 10.1016/j.drugalcdep.2016.01.017. Epub 2016 Jan 29.)
Significance: This study identifies collapsin response mediator protein-2 (CRMP-2) as the convergent point of two independent signaling pathways mediated by mammalian target of rapamycin complex 1 (mTORC1) activation and glycogen synthase kinase-3β (GSK-3β) inhibition associated with excessive alcohol consumption. It is important to note that pharmacologic inhibition of CRMP-2 using an FDA-approved drug or specific knockdown of CRMP-2 levels in the nucleus accumbens attenuates excessive alcohol drinking, suggesting CRMP-2 may be a promising target for the treatment of alcohol-related disorder.
Mammalian target of rapamycin complex 1 (mTORC1) has an essential role in dendritic mRNA translation and participates in mechanisms underlying alcohol-drinking and reconsolidation of alcohol-related memories. Here, we report that excessive alcohol consumption increases the translation of downstream targets of mTORC1, including collapsin response mediator protein-2 (CRMP-2), in the nucleus accumbens (NAc) of rodents. We show that alcohol-mediated induction of CRMP-2 translation is mTORC1-dependent, leading to increased CRMP-2 protein levels. Furthermore, we demonstrate that alcohol intake also blocks glycogen synthase kinase-3β (GSK-3β)-phosphorylation of CRMP-2, which results in elevated binding of CRMP-2 to microtubules and a concomitant increase in microtubule content. Finally, we show that systemic administration of the CRMP-2 inhibitor lacosamide, or knockdown of CRMP-2 in the NAc decreases excessive alcohol intake. These results suggest that CRMP-2 in the NAc is a convergent point that receives inputs from two signaling pathways, mTORC1 and GSK-3β, that in turn drives excessive alcohol-drinking behaviors. (Liu F, Laguesse S, Legastelois R, Morisot N, Ben Hamida S, Ron D. Mol Psychiatry. 8 March 2016; doi:10.1038/mp.2016.12. [Epub ahead of print])
Significance: This study identified calcium/calmodulin-dependent protein kinase II (CaMKII) receptor signaling as a novel target of moderate alcohol drinking that also regulates the positive reinforcing effects of the alcohol in mice. It also demonstrates that CaMKIIα activation increases AMPA receptor activity and that AMPA receptor activity in the amygdala is required for the positive reinforcing effects of alcohol in mice. This indicates that alcohol misappropriates molecular mechanisms of neuroplasticity within the amygdala. This maladaptive activity may represent a molecular gateway from alcohol use to misuse.
Despite worldwide consumption of moderate amounts of alcohol, the neural mechanisms that mediate the transition from use to abuse are not fully understood. Here, we conducted a high-throughput screen of the amygdala proteome in mice after moderate alcohol drinking (n = 12/group) followed by behavioral studies (n = 6-8/group) to uncover novel molecular mechanisms of the positive reinforcing properties of alcohol that strongly influence the development of addiction. Two-dimensional difference in-gel electrophoresis with matrix assisted laser desorption ionization tandem time-of-flight identified 29 differentially expressed proteins in the amygdala of nondependent C57BL/6J mice following 24 days of alcohol drinking. Alcohol-sensitive proteins included calcium/calmodulin-dependent protein kinase II alpha (CaMKIIα) and a network of functionally linked proteins that regulate neural plasticity and glutamate-mediated synaptic activity. Accordingly, alcohol drinking increased α-amino-3-hydroxy-5-methyl-4-isooxazole receptor (AMPAR) in central amygdala (CeA) and phosphorylation of AMPAR GluA1 subunit at a CaMKII locus (GluA1-Ser831) in CeA and lateral amygdala. Further, CaMKIIα-Thr286 and GluA1-Ser831 phosphorylation was increased in CeA and lateral amygdala of mice that lever-pressed for alcohol versus the nondrug reinforcer sucrose. Mechanistic studies showed that targeted pharmacologic inhibition of amygdala CaMKII or AMPAR activity specifically inhibited the positive reinforcing properties of alcohol but not sucrose. Moderate alcohol drinking increases the activity and function of plasticity-linked protein networks in the amygdala that regulate the positive reinforcing effects of the drug. Given the prominence of positive reinforcement in the etiology of addiction, we propose that alcohol-induced adaptations in CaMKIIα and AMPAR signaling in the amygdala may serve as a molecular gateway from use to abuse. (Salling MC, Faccidomo SP, Li C, Psilos K, Galunas C, Spanos M, Agoglia AE, Kash TL, Hodge CW. Biol Psychiatry. 2016 Mar 15;79(6):430-42.)
Significance: This study validates earlier findings that anaplastic lymphoma kinase (ALK) is associated with alcohol dependence in humans and ethanol responses in mice. It demonstrates that ALK might be a useful pharmacotherapeutic target for treating alcohol dependence. The availability of clinically approved ALK inhibitors for the treatment of cancer raises the possibility of clinical testing in alcohol use disorder patients in the near future.
Anaplastic lymphoma kinase (ALK) is a receptor tyrosine kinase associated with alcohol dependence in humans and behavioral responses to ethanol in mice. To characterize the ability of ALK to control ethanol consumption, we treated mice with the ALK inhibitors TAE684 or alectinib before testing them for binge-like drinking using the drinking in the dark protocol. Mice treated with ALK inhibitors drank less ethanol than controls. In addition, TAE684 treatment abolished ethanol conditioned place preference, indicating that ALK regulates the rewarding properties of ethanol. Because the ventral tegmental area (VTA) is a key brain region involved in the rewarding effects of ethanol, we determined if Alk expression in the VTA is important for binge-like ethanol consumption. Mice expressing a short hairpin ribonucleic acid targeting Alk in the VTA drank less ethanol compared with controls. ALK is expressed on dopamine (DA) neurons in the VTA, suggesting that ALK might regulate their firing properties. Extracellular recordings of putative DA neurons in VTA slices demonstrated that ALK inhibition did not affect the ability of ethanol to stimulate, or DA to inhibit, the firing of DA neurons. However, inhibiting ALK attenuated the time-dependent reversal of inhibition produced by moderate concentrations of DA, suggesting that ALK affects DA D2 autoreceptor (D2R) desensitization. Altered desensitization of the D2R changes the firing of DA neurons and is predicted to affect DA levels and alcohol drinking. These data support the possibility that ALK might be a novel target of pharmacotherapy for reducing excessive alcohol consumption. (Dutton JW 3rd, Chen H, You C, Brodie MS, Lasek AW. Addict Biol. 2016 Jan 11. doi: 10.1111/adb.12358.)
Significance: Although alcohol use disorder (AUD) and depression are highly comorbid, treatment options for individuals with both conditions are lacking, and mouse models of alcohol-induced depressive-like behavior have not been well established. This study demonstrates long-lasting depression-like behavior associated with protracted abstinence from alcohol drinking in female mice. This affective disturbance can be reversed by both the n-methyl D-aspartate (NMDA) receptor antagonist, ketamine, and by a monoacylglycerol (MAG) lipase inhibitor, JZL-184, suggesting potentially two distinct pharmacological strategies for the treatment of alcohol-withdrawal-induced mood disorder.
Although alcoholism and depression are highly comorbid, treatment options that take this into account are lacking, and mouse models of alcohol (ethanol (EtOH)) intake-induced depressive-like behavior have not been well established. Recent studies utilizing contingent EtOH administration through prolonged two-bottle choice access have demonstrated depression-like behavior following EtOH abstinence in singly housed female C57BL/6J mice. In the present study, we found that depression-like behavior in the forced swim test (FST) is revealed only after a protracted (2 weeks), but not acute (24 h), abstinence period. No effect on anxiety-like behavior in the EPM was observed. Further, we found that, once established, the affective disturbance is long-lasting, as we observed significantly enhanced latencies to approach food even 35 days after ethanol withdrawal in the novelty-suppressed feeding test (NSFT). We were able to reverse affective disturbances measured in the NSFT following EtOH abstinence utilizing the N-methyl D-aspartate receptor (NMDAR) antagonist and antidepressant ketamine but not memantine, another NMDAR antagonist. Pretreatment with the monoacylglycerol (MAG) lipase inhibitor JZL-184 also reduced affective disturbances in the NSFT in ethanol withdrawn mice, and this effect was prevented by co-administration of the CB1 inverse agonist rimonabant. Endocannabinoid levels were decreased within the BLA during abstinence compared with during drinking. Finally, we demonstrate that the depressive behaviors observed do not require a sucrose fade and that this drinking paradigm may favor the development of habit-like EtOH consumption. These data could set the stage for developing novel treatment approaches for alcohol-withdrawal-induced mood and anxiety disorders. (Holleran KM, Wilson HH, Fetterly TL, Bluett RJ, Centanni SW, Gilfarb RA, Rocco LE, Patel S, Winder DG. Neuropsychopharmacology. 2016 Jan 11. doi: 10.1038/npp.2016.3.)
Endocannabinoid modulation of orbitostriatal circuits gate habit formation
Significance: Difficulty shifting from habit-driven to goal-directed behavior underlies numerous neuropsychiatric disorders including addiction. Understanding of the specific molecular mechanisms and neurocircuitry involved in behavioral shifting is limited, however. This study suggests that the emergence of habitual behavior depends on endocannabinoid-mediated attenuation of activity in an orbitostriatal circuit necessary for goal-directed action.
Everyday function demands efficient and flexible decision-making allowing for habitual and goal-directed action control. An inability to shift has been implicated in disorders with impaired decision-making including obsessive-compulsive disorder and addiction. Despite this, our understanding of specific molecular mechanisms and circuitry involved in shifting action control remains limited. Here we identify an endogenous molecular mechanism, in a specific cortical-striatal pathway, mediating the transition between goal-directed and habitual action strategies. Deletion of cannabinoid type 1 (CB1) receptors from cortical projections originating in the orbitofrontal cortex (OFC) prevents mice from shifting from goal-directed to habitual instrumental lever-pressing. Activity of OFC neurons projecting to dorsal striatum (OFC-DS) and specifically, activity of OFC-DS terminals, is necessary for goal-directed action control. Lastly, CB1 deletion from OFC-DS neurons prevents the shift from goal-directed to habitual action control. These data suggest that the emergence of habits depends on endocannabinoid-mediated attenuation of a competing circuit controlling goal-directed behaviors. (Gremel CM, Chancey J, Atwood B, Luo G, Neve R, Ramakrishnan C, Deisseroth K, Lovinger DM, Costa RM. Neuron, 2016 May 26. pii: S0896-6273(16)30157-X. doi:10.1016/j.neuron.2016.04.043. [Epub ahead of print].)
The Impact of Therapists’ Words on the Adolescent Brain: In the Context of Addiction Treatment
Significance: Studies indicate that therapists’ use of more skillful motivational interviewing techniques, such as encouraging patients to engage in complex reflections about their substance use, may be more likely to result in positive behavior change than the use of less skillful techniques, such as asking closed questions (e.g., those that would elicit a yes/no response). In this study, binge-drinking youth showed clinically significant decreases in their quantity and frequency of drinking after just two therapy sessions, and this change was correlated with brain activation in response to therapist language (i.e., language prompting complex reflections vs. closed questions). These data provide support for the notion that neuroimaging data collected prior to or in response to treatment might be used to predict treatment outcomes.
At this time, we still do not know how therapist behaviors influence adolescent brain response and related treatment outcomes. Therefore, we examined this question with 17 binge drinking youth (mean age=16.62 years; 64.3% female; 42.9% Hispanic; 28.6% bi-/multi-racial). In this within-subjects design, all youth completed a baseline assessment, two therapy sessions, an fMRI scan, and were re-evaluated for behavior change at one-month post-treatment. During the fMRI session, youth were presented with two types of responses from their treating therapist: higher-skill statements prescribed in an empirically-supported addiction treatment (complex reflections) vs. language standard within addiction treatment more broadly (closed questions). In terms of behavior change, at the one-month follow-up, youth showed significant reductions in number of drinking days and binge drinking days. Further, we found main effects for complex reflections and closed questions across the superior middle temporal gyrus and middle temporal gyrus (FWE-corrected, p<.05). Greater brain response was observed for complex reflections versus closed questions within the bilateral anterior cingulate gyrus. Greater BOLD response in the parietal lobe during closed questions was significantly associated with less post-treatment drinking. Lower BOLD response during complex reflections and closed questions in the precuneus were associated with greater post-treatment ratings of importance of changing. This study represents a first step in understanding how therapist behaviors influence the developing adolescent brain and how that neural response may be associated with youth treatment outcomes. (Feldstein Ewing SW, Houck JM, Yezhuvath U, Shokri-Kojori E, Truitt D, Filbey FM, Behav Brain Res. 2016 Jan 15;297:359-69. doi: 10.1016/j.bbr.2015.09.041. Epub 2015 Oct 9.)
Significance: Recent studies suggest that varenicline, an α4β2-nicotinic partial agonist widely used for smoking cessation, can help individuals with alcohol use disorder (AUD) reduce drinking, but the neurocognitive underpinnings of its effectiveness remain largely unexplored. This study demonstrates that varenicline blunts the brain response in the amygdala to negative emotion facial expression images in heavy drinkers suggesting a normalizing of emotional responsivity. Further, this neural response correlated with the number of drinks participants consumed in the last 90 days. This study highlights the utility of the neuroimaging measures of negative emotion response as brain biomarkers of the effectiveness of novel (or repurposed) medications for treating AUD.
BACKGROUND: Pharmacotherapies for alcohol use disorder have been shown to reduce hazardous drinking and improve overall health. The effect sizes for the effectiveness of these medications, however, are small, underscoring the need to expand the range of therapeutics and develop personalized treatment approaches. Recent studies have suggested that varenicline, an α4β2-nicotinic partial agonist widely used for smoking cessation, can help alcoholics reduce drinking, but the neurocognitive underpinnings of its effectiveness remain largely unexplored. METHODS: In this double-blind study, 32 heavy drinkers were randomized to receive varenicline (2 mg/d) or placebo. After 2 weeks of dosing, participants underwent functional MRI scans, during which they viewed images of faces with either neutral or fearful expressions at baseline and following an intravenous alcohol infusion to a target breath alcohol concentration of 80 mg%. Blood oxygen level-dependent (BOLD) response was analyzed with Analysis of Functional Neuroimaging software. Linear mixed-effects models were used to examine the effects of facial expression (fearful vs. neutral) and medication (placebo vs. varenicline) on BOLD response. The effect of medication on measures of subjective response to alcohol was also examined. RESULTS: Results indicated a significant facial expression-by-medication interaction in the left amygdala. The groups showed equivalent activation to neutral faces, but, whereas the placebo group showed increased activation to fearful faces, the varenicline group showed no change in activation. Amygdala activation to fearful faces correlated with number of drinks in the previous 90 days and Obsessive Compulsive Drinking Scale scores. There was no effect of varenicline on subjective response to alcohol. CONCLUSIONS: Our results indicate that varenicline may disrupt amygdala response to fearful faces in heavy drinkers. Further, amygdala activation correlated with alcohol consumption, suggesting that the effects of varenicline may be related to aspects of drinking behavior. These results suggest that amygdala response to fearful faces may be developed as a biomarker of the effectiveness of medications being developed for the treatment of alcohol use disorder. (Gowin JL, Vatsalya V, Westman JG, Schwandt ML, Bartlett S, Heilig M, Momenan R, Ramchandani VA. Alcohol Clin Exp Res. 2016 Apr 8. doi: 10.1111/acer.13046. [Epub ahead of print])
Significance: This article reviews the efficacy and safety of potential medications for the treatment of alcohol use disorder. This includes medications that have shown efficacy with side effects that are mild to moderate in intensity; others that have mixed or promising results but are awaiting findings from ongoing studies; and still others that show poor efficacy, despite promising preliminary results.
Abstract: Alcohol use disorder (AUD), as currently defined in the Fifth Edition of the Diagnostic and Statistical Manual (DSM–5), is a heterogeneous disorder stemming from a complex interaction of neurobiological, genetic, and environmental factors. As a result of this heterogeneity, there is no one treatment for AUD that will work for everyone. During the past two decades, efforts have been made to develop a menu of medications to give patients and clinicians more choices when seeking a therapy that is both effective and which has limited side effects. To date, three medications have been approved by the U.S. Food and Drug Administration (FDA) to treat alcohol dependence: disulfiram, naltrexone, and acamprosate. In addition to these approved medications, researchers have identified new therapeutic targets and, as a result, a number of promising medications are now being evaluated for treatment of AUD in human studies. Although not approved by the FDA for the treatment of AUD, in some cases, these alternative medications are being used off-label by clinicians for this purpose. These potential medications are reviewed here. They include nalmefene, varenicline, gabapentin, topiramate, zonisamide, baclofen, ondansetron, levetiracetam, quetiapine, aripiprazole, and serotonin reuptake inhibitors. The effectiveness of these medications has been mixed—some show good efficacy with side effects that are mild to moderate in intensity, others have mixed or promising results but are awaiting findings from ongoing studies, and still others show poor efficacy, despite promising preliminary results. Medications development remains a high priority. Key initiatives for the National Institute on Alcohol Abuse and Alcoholism (NIAAA) include supporting the discovery and development of more effective and safer medications, advancing the field of personalized medicine, and forging public and private partnerships to investigate new and more effective compounds. (Litten RZ, Wilford BB, Falk DE, Ryan ML, Fertig JB. Subst Abus. 2016, Apr-Jun;37(2):286-98. doi:10.1080/08897077.2015.1133472.)
Significance: Medication development, especially for a disorder as complex as alcohol use disorder (AUD), is challenging and involves multiple phases, including discovery of “druggable” targets, preclinical studies, human clinical trials, and the adoption and implementation of new medication into mainstream medicine. This articles describes the phases of medication development as they apply to AUD, and specific goals of each phase for the next decade.
Abstract: For more than 25 years, advances have been made in developing medications to treat alcohol use disorder (AUD), highlighted by the U.S. Food and Drug Administration’s (FDA’s) approval of naltrexone (oral and long-acting) and acamprosate. Despite this progress, more work remains to be done in this area because these medications, though effective for some people, do not work for everyone. A high priority for the National Institute on Alcohol Abuse and Alcohol (NIAAA) is to put into place a solid infrastructure to aid in the development of medications that are more effective than those currently available, and with few side effects. Medication development, especially for a disorder as complex as AUD, is challenging and involves multiple phases, including discovery of “druggable” targets, preclinical studies, human clinical trials, and the adoption and implementation of the new medication into mainstream medicine. A successful medications development program requires clearly established goals for each phase to ensure that a candidate compound is not trapped in one particular phase, a condition known as “the valley of death.” In this article, the phases of medication development are described as they apply to AUD, and specific goals of each phase are identified for the next decade. In addition, several important crosscutting themes are outlined for each phase, all of which are essential for advancing medications development. These include identifying and validating screening models and druggable targets, making use of precision medicine, and establishing partnerships among key stakeholders. Our goal in writing this article is to provide a guide on medications development that will aid the alcohol research community in planning, testing, and developing medications for AUD. (Litten RZ, Falk DE, Ryan ML, Fertig JB. Alcohol Clin Exp Res. 2016 May 17. Doi: 10.1111/acer.13093. [Epub ahead of print])
Significance: This study examined treatment-seeking alcohol-dependent inpatients with and without post-traumatic stress disorder (PTSD). Results indicate that those with PTSD have similar consumption but greater severity of alcohol dependence, and that those with PTSD have greater mood and anxiety symptoms and disorder diagnoses. Those with PTSD also have higher levels of neuroticism and aggression. These findings indicate that alcohol-dependent patients with comorbid PTSD represent a distinct and more severe clinical sub-population that could benefit from individualized treatment.
Background: Post-traumatic stress disorder (PTSD) is often comorbid with alcohol dependence (AD), but little is known about the characteristics of AD treatment-seeking inpatients with PTSD. We examined differences between treatment-seeking alcohol dependent inpatients with and without comorbid PTSD. We hypothesized that those with AD and PTSD would have higher levels of: (1) alcohol use and AD severity; (2) anxiety and mood disorders; (3) neuroticism. Methods: Individuals (N=411, mean age = 41.7 ± 10.0 years) with AD were monitored over 30 days in a suburban inpatient alcohol treatment setting. Patients were evaluated to identify AD and comorbid PTSD, mood and anxiety disorders, alcohol use and dependence severity, personality, and aggression. Results: Those with PTSD (19% of the sample) did not differ in the amount of alcohol consumed, but had greater: (1) severity of AD (p = 0.001, d = 0.44); (2) diagnosis of anxiety (p = 0.000, OR = 3.64) and mood (p = 0.000, OR = 4.83) disorders; and (3) levels of neuroticism (p < 0.001, d = 0.67) and aggression (p < .001, d = 0.81). Conclusions: AD patients with comorbid PTSD present a more severe phenotype across AD severity, frequency of anxiety and mood disorders, and levels of neuroticism and aggression. This group may benefit from concurrent treatment of both AD and PTSD. Future research can investigate neuroticism as a potential treatment target. (Sells JR, Waters AJ, Schwandt ML, Kwako LE, Heilig M, George DT, Ramchandani VA. Drug Alcohol Depend. In press (2016.))
Alcohol-induced Blackouts as Predictors of Other Drinking Related Harms Among Emerging Young Adults
Significance: Alcohol-related blackouts are periods of amnesia that reflect the failure of the brain to record memories of what transpires while drinking. A national study of emerging adults conducted in 2012-2013 found that 29 percent of drinkers one year past high school reported that, in the past six months because of drinking, they forget where they were or what they did. Blackouts were more prevalent among females and those who in the past 30 days used multiple drugs, more frequently binged, were drunk, smoked, had a lower body weight, and lived in college dorms. After controlling for drinking levels, having a blackout was the strongest predictor of most other alcohol problems experienced by respondents in the past six months. Among emerging adults, questions about blackouts could serve as simple screeners for risk of experiencing other alcohol-related harms.
BACKGROUND: Alcohol-related blackouts are periods of amnesia that reflect the failure of the brain to record memories of what transpires while drinking. This paper examined the incidence, predictors, and behavioral correlates of blackouts among emerging adults and examined whether questions about blackouts could serve as better markers of risk for other alcohol related harms than questions about levels of consumption. METHODS: In 2012 to 2013, 1,463 (68%) of 2,140 respondents 1-year past high school reported having consumed alcohol. They were asked whether, in the past 6 months because of drinking, they forgot where they were or what they did. The survey also explored demographics, substance use behaviors, and other alcohol-related problems in the past 6 months. Chi-square and logistic regression analyses explored bivariate and multivariate predictors of blackouts and other alcohol-related problems. RESULTS: Twenty percent of respondents who ever drank alcohol reported a blackout in the past 6 months. Blackouts were more prevalent among females and those who, in the past 30 days, used multiple drugs, more frequently binged, were drunk, smoked, had lower body weight, and lived in college dorms. After controlling for drinking levels, having a blackout was the strongest independent predictor of most other alcohol problems examined, including in the past 6 months because of drinking, missing class or work, getting behind in work or school, doing something respondents later regretted, arguing with friends, experiencing an overdose, and total number of alcohol problems reported. It was also an independent predictor of hangovers, damaging property, getting hurt, and trouble with police.
CONCLUSIONS: Because blackouts indicate drinking at levels that result in significant cognitive and behavioral impairment, questions about blackouts could serve as important, simple screeners for the risk of experiencing other alcohol related harms. Additional work on this subject is warranted. (Hingson R, Zha W, Simons-Morton B, White A. Alcohol Clin Exp Res. 2016 Apr;40(4):776-84.)
Significance: This study used a computer-administered assessment to examine alcohol involvement, including patterns of alcohol consumption and presence of Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) alcohol use disorder (AUD) in a large sample of adolescents seen in rural primary care settings. The study found that 10 percent of these youth over age 14 years have a past-year DSM-5 AUD. When they examined various alcohol use patterns in this population as a screen for DSM-5 AUD, the researchers found that a single question on past year drinking frequency with age-stratified cut-offs, as recommended in NIAAA’s Alcohol Screening and Brief Intervention for Youth: A Practitioner’s Guide, performs very well.
OBJECTIVE: To examine the National Institute on Alcohol Abuse and Alcoholism Youth Guide alcohol frequency screening thresholds when applied to Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) diagnostic criteria, and to describe alcohol use patterns and alcohol use disorder (AUD) characteristics in rural youth from primary care settings. STUDY DESIGN: Adolescents (n = 1193; ages 12 through 20 years) visiting their primary care practitioner for outpatient visits in six rural primary care clinics were assessed prior to their practitioner visit. A tablet computer collected youth self-report of past-year frequency and quantity of alcohol use and DSM-5 AUD symptoms. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were determined. RESULTS: For early adolescents (ages 12 through 14 years), 1.9% met DSM-5 criteria for past-year AUD and ≥3 days with alcohol use in the past year yielded a screen for DSM-5 with optimal psychometric properties (sensitivity: 89%; specificity: 95%; PPV: 37%; NPV: 100%). For middle adolescents (ages 15 through 17 years), 9.5% met DSM-5 AUD criteria, and ≥3 past year drinking days showed optimal screening results (sensitivity: 91%; specificity: 89%; PPV: 50%; NPV: 99%). For late adolescents (ages 18 through 20 years), 10.0% met DSM-5 AUD criteria, and ≥12 past year drinking days showed optimal screening results (sensitivity: 92%; specificity: 75%; PPV: 31%; NPV: 99%). The age stratified National Institute on Alcohol Abuse and Alcoholism frequency thresholds also produced effective results. CONCLUSION: In rural primary care clinics, 10% of youth over age 14 years had a past-year DSM-5 AUD. These at-risk adolescents can be identified with a single question on alcohol use frequency. (Clark DB, Martin CS, Chung T, Gordon AJ, Fiorentino L, Tootell M, Rubio DM. J. Pediat. 2016 Jun; 173:214-20. doi: 10.1016/j.jpeds.2016.02.047.)
Press and Publications Activities:
Recent News Media Interviews
Dr. Koob continues to speak with a variety of national and international news outlets on timely topics related to NIAAA’s research and its impact on treatment and prevention of alcohol abuse and AUDs. Notable interviews since February include the Washington Post, Boston Globe, Philadelphia Inquirer, Wall Street Journal, and El Paso Times.
Publication Statistics
As of the end of April 2016, there were 31,186 subscribers to the Alcohol Alert; 30,666 to Alcohol Research: Current Reviews; 20,039 to the NIAAA Spectrum; and 19,699 to receive general information.
Press Releases
Study supports single-question alcohol screen for adolescents (April 6, 2016)
Students Explore the Brain with NIH Scientists - NIH celebrates Brain Awareness Week 2016 (March 11, 2016)
Marijuana use disorder is common and often untreated (March 4, 2016)
Criminal justice alcohol program linked to decreased mortality (February 10, 2016)
NIAAA selects winners of its Wearable Alcohol Biosensor Challenge (May 19, 2016)
Coming this week, release on Endocannabinoid Modulation of Orbitostriatal Circuits Gate Habit Formation
Partnerships, Outreach & Public Liaison Activities:
U.S.A. Science and Engineering Festival (USASEF)
The U.S.A. Science and Engineering Festival (USASEF) was held on April 15–17, 2016, at the Walter E. Washington Convention Center in Washington, D.C. As part of the NIH Pavilion, NIAAA staff hosted the “Cool Spot Carnival,” where participants tossed a ball while wearing Fatal Vision goggles to simulate the effects of alcohol on coordination. The NIH Pavilion had an estimated 50,000 visitors this year.
Alcohol Awareness Month
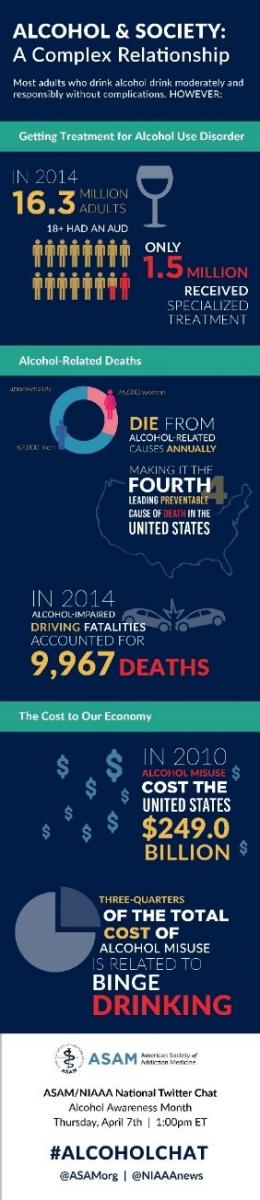
 To commemorate Alcohol Awareness Month, NIAAA tweeted messages on prevalence, symptoms, and treatment of AUD throughout April 2016, using the #AlcoholAwareness hashtag.
To commemorate Alcohol Awareness Month, NIAAA tweeted messages on prevalence, symptoms, and treatment of AUD throughout April 2016, using the #AlcoholAwareness hashtag.
NIAAA also partnered with ASAM for a chat as part of NIAAA’s Alcohol Awareness Month outreach activities. ASAM and NIAAA collaborated on an infographic (pictured right) used during the chat that will be displayed widely as a banner at a variety of meetings and conferences. The chat addressed the science of addiction, current evidence-based approaches for treating alcohol use disorder, and resources for health professionals. Dr. Aaron White served as the scientific expert. The chat had an estimated reach of 275,000 Twitter users and is archived at https://storify.com/NIAAAnews/alcohol-awareness-month-chat-niaaa-and-asam
Social Media:
Twitter Messages & Graphics – St. Patrick’s Day

NIAAA tweeted St. Patrick’s Day-themed messages leading up to the holiday. Enhanced outreach effort resulted in the images being shared or retweeted by the Office of Women’s Health, local TV news affiliates, ABC Health News Chief Dr. Richard Besser, men’s lifestyle and travel blogger James Hill, addiction coach Dr. Cali Estes, and best-selling author Sarah Dessen. People.com also ran the images at no cost on its website, receiving 326,000 impressions. All social media outreach had a potential audience of 1.9 million followers.
Twitter Messages & Graphics – Super Bowl
Leading up to the Super Bowl on February 7, 2016, NIAAA reached out with two alcohol-related social media images: “Don’t Get Sacked” and “Time to Punt.” As a result of enhanced outreach efforts, the messages were shared by Men’s Health Magazine, CBS New York, WFAN New York Radio, and other social media influencers such as ABC News Chief Dr. Richard Besser, radio host Marilyn Russell, and WKYC Senior Health Correspondent Monica Robins. People.com also ran the images at no cost on its website through Super Bowl weekend. Together, the potential social media reach was 4.6 million users.
Other Twitter Messages and Graphics
NIAAA also used its social media presence (@NIAAAnews currently has more than 14,700 followers on Twitter) to publicize various other significant events, including National Children of Alcoholics Week and health messages during spring break.
Blue Pencil Awards:
The NIAAA publication Treatment for Alcohol Problems: Finding and Getting Help was selected to receive a prestigious Blue Pencil Award from the National Association of Government Communicators (NAGC).The publication received the highest marks possible for “fulfilling its purpose, goal or objective” and for writing that is clear, concise, and correct for its intended audience. Judges remarked that the publication is a “well-written and easy-to-read informational product.” The publication is available at http://pubs.niaaa.nih.gov/publications/Treatment/treatment.htm.
 NIAAA was also recognized for the success of its New Year's Eve outreach efforts, receiving a 2015 Blue Pencil/Gold Screen Award in the category of Social Media. This outreach focused on promoting NIAAA’s videopublic service announcement (PSA) titled, “Rethink Your Holiday Drinking” (see http://bit.ly/1J344cj), and also encouraged people to visit NIAAA’s website RethinkingDrinking.niaaa.nih.gov for resources on low-risk drinking around the holidays.
NIAAA was also recognized for the success of its New Year's Eve outreach efforts, receiving a 2015 Blue Pencil/Gold Screen Award in the category of Social Media. This outreach focused on promoting NIAAA’s videopublic service announcement (PSA) titled, “Rethink Your Holiday Drinking” (see http://bit.ly/1J344cj), and also encouraged people to visit NIAAA’s website RethinkingDrinking.niaaa.nih.gov for resources on low-risk drinking around the holidays.
Website – New Content:
A New College Alcohol Intervention Matrix (CollegeAIM) video posted on the NIAAA website, “Targeting Harmful and Underage Student Drinking with NIAAA's CollegeAIM”:
http://niaaa.nih.gov/targeting-harmful-and-underage-student-drinking-niaaas-collegeaim.
Selected Presentations:
NIAAA supported a series of presentations that National Organization on Fetal Alcohol Syndrome (NoFAS) gave to students at the Georgetown University School of Nursing and Health Sciences. The presentations consisted of NIAAA-sponsored research related to FASD and AUD.
CollegeAIM Presentations: NIAAA continues to publicize CollegeAIM, a tool to help colleges to select evidence-based approaches to address problem student drinking. These include presentations at the following events:
-
- CADCA 26th Annual National Leadership Forum on February 3, 2016. The presentation was given by Jason Kilmer, Ph.D., Assistant Director of Health and Wellness for Alcohol and Other Drug Education, University of Washington. More than 60 participants from coalitions around the country attended.
-
- PaperClip Communications Higher Education Webinar on February 18, 2016. NIAAA and PaperClip Communications co-hosted a webinar to discuss CollegeAIM. Presentations were given by George F. Koob, Ph.D., NIAAA Director; Jonathan Gibralter, Ph.D., President, Wells College, and chair of the NIAAA College Presidents Working Group to Address Harmful and Underage College Drinking; and Jason Kilmer, Ph.D. Approximately 20 schools participated.
- American College Health Association conference on May 31–June 4, 2016, in San Francisco, California. The presentation was given by Jason Kilmer, Ph.D.
Mendelson and Hughes Award Winners:
-
- Mendelson: Marlene Oscar Berman, Ph.D., delivered this year’s Jack Mendelson Honorary Lecture on May 25, 2016. Dr. Berman was honored for advancing our understanding of the brain mechanisms underlying the perceptual, emotional, and cognitive impairments associated with chronic alcohol use disorder over her 40-year career as a researcher and educator. The purpose of the Jack Mendelson Honorary Lecture Series is to highlight clinical/human research by an outstanding investigator who has made significant and long-term contributions to our understanding of alcoholism susceptibility, alcohol’s effects on the brain and other organs, and the prevention and treatment of alcohol use disorder.
- Hughes: General Arthur T. Dean, Chairman and CEO of CADCA, received this year’s Senator Harold Hughes Memorial Award from NIAAA on June 9, 2016. CADCA represents over 5,000 coalitions and affiliates working to make America’s communities safe, healthy, and drug-free. Since 1998, General Dean has shaped CADCA’s vision of community empowerment and service, expanded its services, increased its funding, and served as its primary spokesman. The Hughes Award recognizes the contributions of an individual whose work translates research into practice, and builds bridges across the alcohol prevention, treatment, and policy-making communities.

