NIAAA Director's Report on Institute Activities to the 152nd Meeting of the National Advisory Council on Alcohol Abuse and Alcoholism
Table of Contents
- NIAAA BUDGET
- COLLABORATIVE RESEARCH ON ADDICTION AT NIH (CRAN) UPDATE
- DIRECTOR'S ACTIVITIES
- STAFF TRANSITIONS
- HONORS & AWARDS
- RECENTLY ISSUED NOTICE OF FUNDING OPPORTUNITIES
- NOTABLE NIAAA STAFF ACTIVITIES
- WHAT'S AHEAD?
- NIH RESEARCH HIGHLIGHTS
- NIAAA COMMUNICATIONS ACTIVITIES
Fiscal Year (FY) 2019
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) is currently closing out FY 2019. In FY 2019, the National Institutes of Health (NIH) received a total of $39.3 billion, $2.1 billion above the FY 2018 enacted level. This funding includes allocations for the Helping to End Addiction Long-term (HEAL) Initiative, the 21st Century Cures Act, the Brain Research through Advancing Innovative Neurotechnologies (BRAIN) Initiative, and research on influenza. The budget provided a general increase to NIH Institutes and Centers and continued support for the Gabriella Miller Kids First Act pediatric research initiative.
The FY 2019 appropriation for NIAAA provided $525.6 million. This represents a $16 million (3.1 percent) increase over the FY 2018 budget level. NIAAA estimates it will support a total of 782 research project grants (RPGs) in FY 2019. In FY 2018, NIAAA supported 738 RPGs.
FY 2020
The FY 2020 budget is still under development.
| MECHANISM |
FY 2019* Enacted |
|
|---|---|---|
| No | Amount | |
| Research Projects | ||
| Noncompeting | 590 | $226,610 |
| Administrative Supplements | (25) | $2,000 |
| Competing | 192 | $66,590 |
| Subtotal, RPGs | 782 | 295,200 |
| SBIR/STTR | 27 | 13,375 |
| Research Project Grants | 809 | 308,575 |
| Research Centers | ||
| Specialized/Comprehensive | 21 | 31,547 |
| Clinical Research | - | - |
| Biotechnology | - | - |
| Comparative Medicine | - | - |
| Res. Centers in Minority Instit. | - | - |
| Subtotal, Centers | 21 | 31,547 |
| Other Research | ||
| Research Careers | 124 | 20,325 |
| Cancer Education | - | - |
| Cooperative Clinical Research | 1 | 7,530 |
| Biomedical Research Support | - | - |
| Minority Biomed. Research Support | 2 | 500 |
| Other | 67 | 17,500 |
| Subtotal, Other Research | 194 | 45,855 |
| Total Research Grants | 1,024 | 385,977 |
| Training | ||
| Individual | 119 | $5,547 |
| Institutional | 176 | $9,578 |
| Total Training | 295 | 15,125 |
| Research & Develop. Contracts | 34,195 | |
| (SBIR/STTR) | (2372) | |
| Intramural Research | $54,412 | |
| Res. Management & Support | $35,607 (10) |
|
| Total, NIAAA Budget Authority | $525,316 | |
*FY2019 Enacted Total: Mandatory transfer amount accounts for the difference of -$275K
COLLABORATIVE RESEARCH ON ADDICTION AT NIH (CRAN) UPDATE
Adolescent Brain Cognitive Development (ABCD) Study
The ABCD Study is continuing to follow the 11,874 participants in the longitudinal study design. Earlier this year, several notice of funding opportunities were issued to continue the ABCD study.
CRAN Mentored K Career Development Workshop
NIAAA, in collaboration with the National Institute on Drug Abuse (NIDA) and the National Cancer Institute (NCI), sponsored the First Biennial CRAN Mentored Career Development Workshop on August 13–14, 2019. Held on campus at the John Edward Porter Neuroscience Research Center, this two-day workshop supported mentored career (K) awardees to provide information and guidance on grant writing, research, funding priorities and networking opportunities to help advance and sustain successful independent research careers. NIAAA supported 40 K-awardees from the 129 total participants. Lynn Morin represented NIAAA on the organizing committee for this workshop. Several NIAAA Program, Review, and Grants Management staff attended and were available to meet with the junior investigators in dedicated sessions. Dr. Nora Volkow, NIDA Director, opened the Tuesday session with a presentation about NIDA priorities and opportunities and Dr. George F. Koob, NIAAA Director, opened the Wednesday session with a presentation about NIAAA priorities and opportunities. Dr. Abraham Bautista, Director of NIAAA’s Office of Extramural Activities, provided an overview of grants available to new and early stage investigators.
NIAAA Director Dr. George F. Koob made the following plenary presentations between April 1, 2019, and July 31, 2019:
- “NIAAA’s Efforts to Increase Treatment for Alcohol Use Disorder” for the American College of Academic Addiction Medicine in Orlando, Florida, on April 3, 2019
- “The Emotional Pain of Addiction: Hyperkatifeia, Negative Reinforcement and New Targets for Treatment” at the American Society of Addiction Medicine Annual Conference in Orlando, Florida, on April 5, 2019
- “Drug Addiction: The Gain in the Brain is in the Pain” at the 13th Annual Undergraduate Research Symposium at William Paterson University in Wayne, New Jersey, on April 6, 2019
- “The Negative Emotional Side of Drug Addiction: From Drug Reward to Hyperkatifeia to Negative Reinforcement” at the 25th Annual Wisconsin Symposium on Emotion in Madison, Wisconsin, on April 10, 2019
- “NIH Training Opportunities: Engaging the Next Generation of Scientists” at the American Psychiatric Association Annual Meeting in San Francisco, California, on May 19, 2019
- “What Science Can Tell about the Treatment of Alcohol Use Disorders” at the Annual Meeting of the American Society of Clinical Psychopharmacology in Scottsdale, Arizona, on May 20, 2019
- “NIAAA Update” for the Friends of NIAAA Annual Meeting in Washington, DC, on May 22, 2019
- “Neurobiology of Addiction: The Gain in the Brain is in the Pain” at the World Congress of Biological Psychiatry Conference in Vancouver, Canada, on June 4, 2019
- “A Heuristic Domain Framework for Understanding the Prevention, Diagnosis, and Treatment of Alcohol Use Disorders” at the 81st Annual Meeting of the College on Problems of Drug Dependence in San Antonio, Texas, on June 16, 2019
- “NIAAA Update” at the Annual Research Society on Alcoholism Scientific Meeting in Minneapolis, Minnesota, on June 23, 2019
- “Remember Ting-Kai Li: Perspectives from an NIAAA Director” at the Annual Research Society on Alcoholism Scientific Meeting in Minneapolis, Minnesota, on June 24, 2019
- “Drug Addiction: From Drug Reward to Hyperkatifeia to Negative Reinforcement” at the 29th Annual International Cannabinoid Research Society Symposium on the Cannabinoids in Bethesda, Maryland, on July 1, 2019
- “Alcohol and Drug Addiction: The Gain in the Brain is in the Pain” at the International Narcotics Research 50th Anniversary Meeting in New York, New York, on July 9, 2019
- “Neurobiology of Alcohol Use Disorder: A Heuristic Framework for Future Research” at the Fourth International Conference on Applications of Neuroimaging to Alcoholism at Yale University in New Haven, Connecticut, on July 19, 2019
- “Alcohol and Drug Addiction: The Gain in the Brain is in the Pain” at the University of California San Diego on July 25, 2019, in San Diego, California
New Staff

Gabriela Coello joined the Administrative Services Branch as an Administrative Officer supporting the intramural laboratories of Drs. David Goldman, Hee-Yong Kim, Pal Pacher, and Richard Veech. She previously worked at the National Cancer Institute.

Dr. Yong He joined the Laboratory of Liver Diseases (LLD) as a Research Fellow in the Visiting Program. He previously served in the NIH Graduate Partnership Program in LLD. He received his Ph.D. in Pharmacology from Anhui Medical University in Hefei, China. Dr. He will be working on two projects during the coming year. The first one involves a mouse model of nonalcoholic steatohepatitis induced by a high-fat diet to assess the pathogenic role of miRNA-223 and the therapeutic potential of miR-223 as a target to treat nonalcoholic steatohepatitis. The second project is to explore the function of interleukin-20 in the pathogenesis of liver diseases in several models including Con A-induced hepatitis and bacterial infection.

Cassie Williams joined the Administrative Services Branch as an Administrative Officer supporting the intramural laboratories of Drs. David Lovinger, Steven Vogel, and Klaus Gawrisch. She previously worked at the National Institute of Allergy and Infectious Diseases.
Internal Transitions

Dr. Tatiana Balachova joined the NIAAA Division of Epidemiology and Prevention Research as a Senior Scientific Administrator and was appointed Scientific Coordinator and Executive Secretary of the Interagency Coordinating Committee on Fetal Alcohol Spectrum Disorders. She was previously a Senior Scientist at NIAAA through the Intergovernmental Personnel Act (IPA) Mobility Program from the University of Oklahoma Health Sciences Center (OUHSC), where she was Professor of Pediatrics and Co-Director of the Interdisciplinary Training Program in Child Abuse and Neglect. Dr. Balachova earned a Doctor of Philosophy in Clinical Psychology and Psychiatry/Substance Abuse from the Bekhterev Research Psychoneurological Institute in Leningrad, Russia, and completed postdoctoral training in pediatric psychology and child abuse and neglect at OUHSC in 2001. Her areas of research interest include fetal alcohol spectrum disorders, child maltreatment, HIV/AIDS, and health risk behaviors. She will be administrating grants on the following topics: reproductive and perinatal epidemiology, prevention among women of child-bearing age, family-based prevention, and HIV/AIDS prevention.

Dr. Svetlana Radaeva was selected as the Deputy Director of NIAAA’s Division of Metabolism and Health Effects (DMHE). Dr. Radaeva obtained her Ph.D. in Cell Biology from the Institute of Developmental Biology, USSR Academy of Sciences in Moscow, Russia. She has trained in hepatology at the Deutsches Krebsforschungszentrum (DKFZ), German Cancer Research Center in Heidelberg, Germany, and at Virginia Commonwealth University in Richmond, Virginia. From 2000–2006, she held a Staff Scientist position in NIAAA’s Section on Liver Biology, where her work focused on the role of the innate immunity in alcohol-associated hepatic injury, repair, and fibrosis. Dr. Radaeva has served as Program Officer within DMHE since 2006, overseeing a portfolio on alcohol-associated liver disease and serving as NIAAA representative on the Coordinating Committee for Research on Women’s Health (CCRWH ) and Trans-NIH Rare Disease working group. Dr. Radaeva’s areas of expertise include ultrastructural morphology of chronic liver disease, hepatic progenitor cell proliferation, hepatocarcinogenesis, and clinical trial project management

Dr. Mehdi Farokhnia was promoted from Postdoctoral Intramural Research Training Award (IRTA) Fellow in the NIAAA/NIDA Section on Clinical Psychoneuroendocrinology and Neuropsychopharmacology (CPN) to Research Fellow in CPN. Dr. Farokhnia received his M.D. from Tehran University of Medical Sciences in 2012, where he received training in the neurobiology of mental health disorders and testing of potential medication candidates through phase II and III clinical trials. His research in CPN has focused on identifying novel druggable targets, through a combination of pharmacological, behavioral, genetic, and neuroimaging methods, to treat alcohol use disorder. He is also interested in investigating human laboratory approaches that may best translate preclinical findings into clinical research and facilitate the medications development pipeline, with a particular focus on neurobehavioral pharmacology and substance use.

Dr. Laura Kwako transitioned from her role as Clinical Research Psychologist in the NIAAA intramural Office of the Clinical Director to Program Officer in the Division of Treatment and Recovery Research. Her research portfolio focuses on health services, including treatment availability, quality, and use, along with health care systems and integration of various health care services. Dr. Kwako received her Ph.D. in Clinical Psychology from the Catholic University of America and completed postdoctoral clinical training at Springfield Hospital Center in Maryland, specializing in treatment for addiction and trauma-related disorders.

Dr. Rachel Anderson transitioned from her role as an American Association for the Advancement of Science (AAAS) Science and Technology Policy Fellow to Health Science Policy Analyst in the Science Policy Branch of NIAAA’s Office of Science Policy and Communications. She previously served as an AAAS Fellow at the National Institute of Justice within the Department of Justice, where she provided programmatic support for multiple criminal justice research initiatives while studying alcohol and drug policy. Dr. Anderson earned her Ph.D. in Behavioral Neuroscience at Binghamton University where her research examined developmental differences in alcohol sensitivity. She also studied interactions of stress and alcohol dependence as a postdoctoral fellow at the Medical University of South Carolina.
Departing Staff
Erin Bryant, who served as a Science Writer and Social Media Strategist in the Communications and Public Liaison Branch, has moved to the NIH Office of the Director, where she now works as a Technical Writer for NIH Research Matters and NIH News in Health.
Yolanda Carter, Administrative Laboratory Manager with Laboratory of Integrative Neuroscience, moved to the NIH Office of Research Facilities.
Dr. Abhishek Desai completed his fellowship in the Laboratory of Molecular Signaling and is currently spending time with his family.
Dr. Lori Ducharme, former Program Director in the Division of Treatment and Recovery Research, transferred to the National Institute on Drug Abuse where she now serves as Health Scientist Administrator in the Services Research Branch.
Lynn Morin, former Chair of the Centers and Training Working Group and Diversity Supplement Program Coordinator for the NIAAA Office of Extramural Activities, transferred to the NIH Office of Research on Women’s Health after eight years of service at NIAAA.
Monte Philips, Biologist in the Section on Clinical Genomics and Experimental Therapeutics, has retired after working in the NIAAA intramural research program for 29 years.
Dr. Richard Rippe, Scientific Review Officer, Extramural Project Review Branch, Office of Extramural Activities, retired after 10 years of federal service. While at NIAAA, he was the Designated Federal Officer for Special Emphasis Panels that reviewed various grant mechanisms, including Individual Fellowship (F) and Institutional Training (T32/T35) grant applications.
Kamilah Smith, Administrative Assistant with the Division of Neuroscience and Behavior, accepted a position as Program Specialist with the Center for Drug Evaluation and Research within the U.S. Food and Drug Administration (FDA).
Dr. Judith Arroyo received the First Annual Dora Goldstein Diversity in the Sciences Award at the annual meeting of the Research Society on Alcoholism in June 2019.
Dr. Mehdi Farokhnia, Research Fellow in the NIAAA/NIDA Section on Clinical Psychoneuroendocrinology and Neuropsychopharmacology, received a Pathways Research Grant funded by the Alkermes Pathways Research Awards Program. He also received a Fellows Award for Research Excellence (FARE) from the NIH.
Dr. George Kunos, Scientific Director of the Division of Intramural Clinical and Biological Research, received the Lifetime Achievement Award from the International Cannabinoid Research Society (ICRS) “for his high impact work on the role of endocannabinoid-cannabinoid 1 receptor signaling in the regulation of cardiovascular function, lipid and carbohydrate metabolism, and demonstration of benefits of peripherally restricted cannabinoid 1 receptor antagonists in obesity, drinking behavior and diabetes, furthering the endocannabinoid research field.” The award was made on July 3, 2019 at the annual meeting of the ICRS in Bethesda, Maryland.
Dr. Daria Piacentino, Visiting Fellow in the NIAAA/NIDA Section on Clinical Psychoneuroendocrinology and Neuropsychopharmacology, was presented with an American Society of Clinical Psychopharmacology New Investigator Award in May 2019. She also received a fellowship from the NIH Center on Compulsive Behaviors.
The following NIAAA staff members received 2019 NIH Director’s Awards, presented on July 15, 2019:
- Dr. Andrew Holmes, Chief of the Laboratory of Behavioral and Genomic Neuroscience, was awarded a Director’s Award in the Scientific/Medical category “in recognition for discovering novel neural mechanisms of learning and drug effects, outstanding leadership in the neuroscience addiction field, and exemplary mentoring skills.”
- Dr. David Lovinger, Deputy Scientific Director of the Division of Intramural Clinical and Biological Research, was awarded a Director’s Award in the Administrative category for his role in helping to “establish the NIH Equity Committee as a forum for identifying and disseminating best practices in intramural research resource allocation”.
- Dr. Kathy Jung, Director of the Division of Metabolism and Health Effects, was awarded a Director’s Award in the Scientific/Medical category for her role in the trans-NIH Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Working Group “in recognition of efforts supporting awareness and activities that advance Myalgic Encephalomyelitis/Chronic Fatigue Syndrome research.”
RECENTLY ISSUED NOTICE OF FUNDING OPPORTUNITIES
Notice of Funding Opportunity (NOFO) Issued by NIAAA
Specialized Alcohol Research Centers (P50 Clinical Trial Optional): This Notice of Funding Opportunity (NOFO) solicits applications for specialized Alcohol Research Centers using the P50 mechanism. The overall purpose of the NIAAA Alcohol Research Center program is to provide leadership in conducting and fostering interdisciplinary, collaborative research on a wide variety of topics relevant to the Institute’s mission. RFA-AA-20-001
Comprehensive Alcohol Research Centers (P60 Clinical Trial Optional): This Notice of Funding Opportunity (NOFO) solicits applications for Comprehensive Alcohol Research Centers using the P60 mechanism which requires a dissemination core to initiate and expand community education related to the activities of the center. The P60 is also expected to provide leadership in conducting and fostering interdisciplinary, collaborative research on a wide variety of topics relevant to the Institute’s mission. RFA-AA-20-002
Mechanisms of Tolerance (R21/R33 Clinical Trial Required): This notice of funding opportunity (NOFO) focuses on sensitivity and tolerance mechanisms underlying the development of alcohol use disorder, specifically, (1) to develop hypotheses about cellular, molecular or network mechanisms that regulate sensitivity and tolerance to alcohol, and (2) to develop quantitative models to predict the development of tolerance and the progression to alcohol use disorder. PAR-19-311
NIH-Wide NOFOs with NIAAA’s Participation
BRAIN Initiative: Non-Invasive Neuromodulation - New Tools and Techniques for Spatiotemporal Precision (R01 Clinical Trial Optional) RFA-MH-20-310
BRAIN Initiative: Proof of Concept Development of Early Stage Next Generation Human Brain Imaging (R01 Clinical Trial Not Allowed) RFA-EB-19-001
BRAIN Initiative: Development of Next Generation Human Brain Imaging Tools and Technologies (U01 Clinical Trial not allowed) RFA-EB-19-002
BRAIN Initiative: Marmoset Coordination Center (U24 Clinical Trials Not Allowed) RFA-MH-20-150
BRAIN Initiative: Marmoset Colonies for Neuroscience Research (U24 Clinical Trials Not Allowed) RFA-MH-20-145
BRAIN Initiative: Research to Develop and Validate Advanced Human Cell-Based Assays To Model Brain Structure and Function (R01 Clinical Trial Not Allowed) RFA-MH-20-140
Secondary Analyses of Existing Datasets of Tobacco Use and Health (R21 Clinical Trial Not Allowed) RFA-OD-19-022
Maximizing the Scientific Value of Existing Biospecimen Collections (R21 Clinical Trial Not Allowed) RFA-OD-19-021
Methods to Improve Reproducibility of Human iPSC Derivation, Growth and Differentiation (SBIR) (R44 Clinical Trial Not Allowed) RFA-GM-19-001
Dissemination and Implementation Research in Health (R01 Clinical Trial Optional) PAR-19-274; (R21 Clinical Trial Optional) PAR-19-275; (R03 Clinical Trial Not Allowed) PAR-19-276
NOTABLE NIAAA STAFF ACTIVITIES
Dr. Judith Arroyo, along with Dr. Kathy Etz from NIDA, presented a preconference workshop focused on “Applying to the NIH to Support Research on Addictive Behaviors across Diverse Populations” at the 2019 Collaborative Perspective on Addiction Meeting in Providence, Rhode Island, on April 4, 2019.
Dr. Ralph Hingson presented at the STOP Act National Stakeholders Meeting on July 31, 2019, hosted by the Interagency Coordinating Committee on the Prevention of Underage Drinking (ICCPUD).
Dr. Kathy Jung provided an introductory presentation on “Cancer-related Research Interests of the National Institute on Alcohol Abuse and Alcoholism (NIAAA)”at the Fourth Alcohol and Cancer Conference in Newport, Rhode Island, on April 14—17, 2019.
Dr. Pal Pacher served as President of the International Cannabinoid Research Society, chaired the scientific programme committee, and organized the 29th Annual Meeting held in Bethesda, Maryland, on June 29—July 4, 2019.
Dr. George Kunos presented a plenary talk titled “Endocannabinoid Signaling via the Gut-Brain Axis: Relevance to Addictive Behaviors” and Dr. David Lovinger presented a talk titled “Chronic THC on Sleep and Monoamine” at the Gordon Research Conference on Cannabinoid Function in the Central Nervous System, in Castelldefels, Spain, in July 2019.
Dr. Lorenzo Leggio presented “The Gut in the Brain: Potential Novel Targets for the Treatment of Addictions” at the NIH Blueprint Workshop, The Science of Interoception and Its Roles in Nervous System Disorders, in Bethesda, Maryland, on April 16—17, 2019.
Dr. Soundar Regunathan served as co-chair and discussion moderator for one of the sessions at a workshop organized by the National Center on Sleep Disorders Research (NHLBI) on Sleep Insufficiency, Circadian Misalignment and the Immune System held in Rockville, Maryland, on May 16—17, 2019.
Dr. Deidra Roach moderated a symposium titled “Problem Drinking Among Medically Underserved Women: New Horizons in Treatment” at the Annual Conference of the American Society of Addiction Medicine in Orlando, Florida, on April 6, 2019.
Dr. Deidra Roach presented a webinar highlighting findings from current research on women and alcohol on behalf of the Interagency Work Group on Drinking and Drug Use in Women and Girls on May 31, 2019.
NIAAA Staff Activities at the 2019 Research Society on Alcoholism (RSA) Annual Meeting, June 22–26, 2019, in Minneapolis, Minnesota:
Satellite Meetings
- Mechanisms of Behavior Change
- “Research Priorities for the Division of Treatment and Recovery Research” – Dr. Raye Litten
- “Mechanisms of Behavior Change in the Treatment of Alcohol Use Disorder: Moving the Dissemination and Implementation Needle Forward” – Dr. Brett Hagman
- "Mechanisms of Behavior Change in the Treatment of Alcohol Use Disorder: An NIAAA Portfolio Update” – Dr. Brett Hagman
- Fetal Alcohol Spectrum Disorder (FASD) Study Group
- “NIAAA Update” – Dr. Bill Dunty
- Participant in roundtable discussion on Career Development – Dr. Bill Dunty
Symposia/Roundtables/Workshops
- “Alcohol and HIV: Building a Global Alcohol Research Agenda for Reproductive Health of People Affected by HIV/AIDs” (Dr. Tatiana Balachova, co-chair and introductory presenter; Dr. Kendall Bryant, co-chair and discussant)
- “The GABA-B Receptor as a Novel Pharmacological Target to Treat Alcohol Use Disorder: Then, Now and the Future” (Dr. Mehdi Farokhnia, speaker; Dr. Lorenzo Leggio, organizer and introductory presenter)
- “Recent Advances in Understanding the Complexity of Alcohol-Induced Pancreatic Dysfunction and Pancreatitis Development” (Dr. Peter Gao, co-chair and discussant)
- “Critical Elements in Adapting Behavioral Treatments for Alcohol Use Disorder among Culturally Sensitive Populations” (Dr. Brett Hagman, discussant)
- “Is the Cuddle Drug for Real? Exploring Oxytocin as a Treatment for Alcohol Use Disorder” (Dr. Mary Lee, speaker; Dr. Lorenzo Leggio, organizer, chair, and discussant)
- “Integrative Approach to Personalized Medicine for Treatment of Alcohol Use Disorder and Associated Psychiatric Disorders” (Dr. Raye Litten; organizer, co-chair, and discussant)
- “Young Scientists Forum on Alcohol-Induced Cellular and Tissue Damage” (Dr. Gary Murray, organizer and co-chair)
- “It’s About Time: Circadian Rhythms and Alcohol-Induced Effects” (Dr. Gary Murray, discussant)
- “Alcohol and The Cardiovascular System: Evolving Concepts In Pathology And Therapy” (Dr. Andras Orosz, co-organizer, co-chair, and discussant)
- “Novel Mechanisms of Cellular Stress and Protein Homeostasis In Alcoholic Organ Injury” (Dr. Andras Orosz, introductory presenter)
- “Advanced Genomic Technologies: Applications to Alcohol Use Disorder” (Dr. Abbas Parsian, co-organizer)
- “Translating Microbiota Research into Clinical Practice for Alcoholic Hepatitis” (Dr. Svetlana Radaeva, co-organizer, co-chair, and introductory presenter)
- “Extracellular vesicles, miRNA, epigenetics and immune signaling in central and peripheral alcoholic pathology” (Dr. Soundar Regunathan, co-chair and introductory presenter)
- “Alcohol and HIV-1 induced pathogenic changes in the gut-liver-brain axis” (Dr. Soundar Regunathan, discussant)
- “Cell-type specific mechanisms of ethanol metabolite action in brain and behavior” (Drs. Li Zhang and Qi-Ying Liu, chairs)
Other RSA Activities
- The RSA Subcommittee of the Centers and Training Working Group, chaired by Dr. Anita Bechtholt, coordinated a number of activities to support early stage investigators and trainees at the meeting. Many NIAAA staff members participated by attending a Meet and Greet, working at the “Ask a Program Officer” table, and hosting one-on-one meetings with trainees and early stage investigators.
- Drs. Amy Fan, Boji Huang, and Tulshi Saha of the Epidemiology and Biometry Branch presented posters on topics including the role of craving in DSM-5 alcohol use disorder criteria and the relationships between alcohol consumption and risks of alcohol use disorder and other adverse health consequences.
NIAAA and NIDA, along with the National Institute on Minority Health and Health Disparities (NIMHD), will again sponsor the National Hispanic Science Network annual meeting on October 9—11, 2019, in New Orleans, Louisiana. In addition to scientific sessions on basic and clinical addiction research, the program includes two invited symposia on alcohol-related research. Dr. Judith Arroyo is the program contact.
Alcoholic and Nonalcoholic Steatohepatitis: Pathogenesis and Mechanisms of Liver Injury Workshop will be held September 16—17, 2019, in Bethesda, Maryland. This research workshop is being jointly sponsored by the NIAAA and the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) with the aim of bringing together research investigators in these two fields and summarizing the current state of the science of various pathophysiological mechanisms that lead to fatty liver injury. A particular focus will be on how the possible pathologic mechanism might be shared or distinct in alcoholic versus nonalcoholic fatty liver disease. Drs. Svetlana Radaeva and Joe Wang are the program contacts.
The Cancer Moonshot Collaborative Meeting (CMCM) will be held November 18—20, 2019, at the Bethesda North Marriott Hotel and Conference Center in Rockville, Maryland. Dr. Gary Murray is the program contact.
NIAAA and NIDA will again sponsor the Frontiers in Addiction Research Mini-Convention on October 18, 2019, as a satellite event to the Society for Neuroscience annual meeting in Chicago, Illinois. In addition to scientific sessions on emerging areas in addiction research, the program will also feature the Jacob Waletzky Memorial Award lecture and Early Career Investigator Showcase. Dr. John Matochik is the program contact.
NIAAA RESEARCH HIGHLIGHTS
Significance: Aldehyde dehydrogenase 2 (ALDH2) is a key enzyme that detoxifies the alcohol metabolite acetaldehyde in the liver. This study demonstrated that ALDH2-deficient mice or humans with chronic liver disease and high alcohol consumption are more susceptible to liver cancer, due to increased production of oxidized mitochondrial DNA-enriched extracellular vesicles that activate multiple oncogenic pathways. Thus, inhibition of oxidized mitochondrial DNA-enriched extracellular vesicle production could be a novel therapeutic strategy for ameliorating alcohol-associated liver cancer in ALDH2-deficient individuals.
Background & Aims: Excessive alcohol drinking is one of the major causes of hepatocellular carcinoma (HCC). Approximately 30-40% Asian population are deficient for aldehyde dehydrogenase 2 (ALDH2), a key enzyme to detoxify the ethanol metabolite acetaldehyde. However, how ALDH2 deficiency affects alcohol-related HCC remains obscure. Methods: ALDH2 polymorphism in 646 patients with viral hepatitis B (HBV) infection with or without alcohol drinking was studied. A new model of HCC induced by chronic carbon tetrachloride (CCl4) and alcohol administration was developed and studied in three lines of Aldh2-deficient mice: including Aldh2 global knockout (KO) mice, Aldh2*1/*2 knock-in mutant mice, and liver-specific Aldh2 KO mice. Results: We demonstrated that ALDH2 deficiency was not associated with liver disease progression but was associated with an increased risk of HCC development in cirrhotic HBV patients with excessive alcohol consumption. The mechanisms underlying HCC development associated with cirrhosis and alcohol consumption were studied in Aldh2-deficient mice. We found that all three lines of Aldh2-deficient mice were more susceptible to CCl4 plus alcohol-associated liver fibrosis and HCC development. Furthermore, our results from in vivo and in vitro mechanistic studies revealed that after CCl4 plus ethanol exposure, Aldh2-deficient hepatocytes produced a large amount of harmful oxidized mtDNA via extracellular vesicles (EVs), which were then transferred into neighboring HCC cells and together with acetaldehyde activated multiple oncogenic pathways (JNK, STAT3, BCL-2, and TAZ), thereby promoting HCC. Conclusions: ALDH2 deficiency is associated with an increased risk of alcohol related-HCC development from fibrosis in patients and in mice. Mechanistic studies reveal a novel mechanism that Aldh2-deficient hepatocytes promote alcohol-associated HCC by transferring harmful oxidized mtDNA-enriched EVs into HCC and subsequently activating multiple oncogenic pathways in HCC. (Seo W, Gao Y, He Y, Sun J, Xu H, Feng D, Hee Park S, Cho YE, Guillot A, Ren T, Wu R, Wang J, Kim SJ, Hwang S, Liangpunsakul S, Yang Y, Niu J, and Gao B. J Hepatol. 2019 Jul 4. pii: S0168-8278(19)30390-3)
Targeting Peripheral CB1 Receptors Reduces Ethanol Intake via a Gut-Brain Axis
Significance: Endocannabinoids and ghrelin are both implicated in promoting alcohol intake, but interactions between the two systems have not been characterized. This study demonstrated that cannabinoid-1 receptor (CB1R) signaling in ghrelin-producing stomach cells modulates the formation of biologically active ghrelin, which then activates a gut-brain signaling pathway that leads to increased alcohol consumption. Peripherally-restricted pharmacological inhibition of CB1R, which avoids the psychiatric side effects of blocking CB1R in the central nervous system, reduced ethanol drinking in mice. Thus, peripheral CB1 receptor blockade may have therapeutic potential in the treatment of alcoholism.
Endocannabinoids acting on the cannabinoid-1 receptor (CB1R) or ghrelin acting on its receptor (GHS-R1A) both promote alcohol-seeking behavior, but an interaction between the two signaling systems has not been explored. Here, we report that the peripheral CB1R inverse agonist JD5037 reduces ethanol drinking in wild-type mice but not in mice lacking CB1R, ghrelin peptide or GHS-R1A. JD5037 treatment of alcohol-drinking mice inhibits the formation of biologically active octanoyl-ghrelin without affecting its inactive precursor desacyl-ghrelin. In ghrelin-producing stomach cells, JD5037 reduced the level of the substrate octanoyl-carnitine generated from palmitoyl-carnitine by increasing fatty acid β-oxidation. Blocking gastric vagal afferents abrogated the ability of either CB1R or GHS-R1A blockade to reduce ethanol drinking. We conclude that blocking CB1R in ghrelin-producing cells reduces alcohol drinking by inhibiting the formation of active ghrelin and its signaling via gastric vagal afferents. Thus, peripheral CB1R blockade may have therapeutic potential in the treatment of alcoholism. (Godlewski G, Cinar R, Coffey NJ, Liu J, Jourdan T, Mukhopadhyay B, Chedester L, Liu Z, Osei-Hyiaman D, Iyer MR, Park JK, Smith RG, Iwakura H, and Kunos G. Cell Metab. 2019 Jun 4;29(6):1320-1333.e8)
Maternal Circulating miRNAs That Predict Infant FASD Outcomes Influence Placental Maturation
Significance: Previous research identified 11 miRNAs in the plasma of pregnant women that predict infant fetal alcohol spectrum disorders (FASD) outcomes following prenatal alcohol exposure (Balaraman S. et al., 2016). In the current report, the same team demonstrated in a mouse model that these miRNAs restrict placental maturation by inhibiting trophoblast epithelial-mesenchymal transition, a key process for development of the placenta. Importantly, in-vitro cell data also supported the potential of targeting these miRNAs for therapeutic intervention. Collectively, these findings suggest that prenatal alcohol results in fetal growth restriction in part by impairing placental function via specific miRNAs.
Prenatal alcohol exposure (PAE), like other pregnancy complications, can result in placental insufficiency and fetal growth restriction, although the linking causal mechanisms are unclear. We previously identified 11 gestationally elevated maternal circulating miRNAs (HEamiRNAs) that predicted infant growth deficits following PAE. Here, we investigated whether these HEamiRNAs contribute to the pathology of PAE, by inhibiting trophoblast epithelial-mesenchymal transition (EMT), a pathway critical for placental development. We now report for the first time that PAE inhibits expression of placental pro-EMT pathway members in both rodents and primates, and that HEamiRNAs collectively, but not individually, mediate placental EMT inhibition. HEamiRNAs collectively, but not individually, also inhibited cell proliferation and the EMT pathway in cultured trophoblasts, while inducing cell stress, and following trophoblast syncytialization, aberrant endocrine maturation. Moreover, a single intravascular administration of the pooled murine-expressed HEamiRNAs, to pregnant mice, decreased placental and fetal growth and inhibited the expression of pro-EMT transcripts in the placenta. Our data suggest that HEamiRNAs collectively interfere with placental development, contributing to the pathology of PAE, and perhaps also, to other causes of fetal growth restriction. (Tseng AM*, Mahnke AH, Wells AB, Salem NA, Allan AM, Roberts VH, Newman N, Walter NA, Kroenke CD, Grant KA, Akison LK, Moritz KM, Chambers CD, and Miranda RC; Collaborative Initiative on Fetal Alcohol Spectrum Disorders. Life Sci Alliance. 2019 Mar 4;2(2). pii: e201800252)
*Denotes NIAAA-funded F trainee
Significance: The negative emotional state associated with alcohol withdrawal is a driving force for alcohol relapse; however, the underlying neurobiological mechanisms are not fully understood. In this study, activation of glycine receptors in the lateral habenula alleviated alcohol withdrawal-induced anxiety- and depression-like behaviors and reduced alcohol consumption in rats. These data, together with recent evidence on the critical role of the lateral habenula in depression, reveal a new mechanism underlying the negative emotional state associated with alcohol withdrawal and a potential therapeutic target for alcohol use disorder.
The lateral habenula (LHb) is activated by a range of aversive states including those related to alcohol withdrawal and has glycine receptors (GlyRs), a sensitive target of alcohol. However, whether GlyRs in the LHb contribute to alcohol-related behaviors is unknown. Here, we report that rats experiencing withdrawal from chronic alcohol consumption showed higher anxiety and sensitivity to stress compared to their alcohol-naïve counterparts. Intra-LHb injection of glycine attenuated these aberrant behaviors and reduced alcohol intake upon alcohol re-access. Glycine's effect was blocked by strychnine, a GlyR antagonist, indicating that it was mediated by strychnine-sensitive GlyRs. Conversely, intra-LHb strychnine elicited anxiety- and depression-like behaviors in Naïve rats but not in withdrawal rats. Additionally, both the frequency and the amplitude of the spontaneous IPSCs were lower in LHb neurons in slices of withdrawal rats compared to naïve rats. Also, there were sporadic strychnine-sensitive synaptic events in some LHb neurons. Bath perfusion of strychnine induced a depolarizing inward current and increased action potential firings in LHb neurons. By contrast, bath perfusion of glycine or sarcosine, a glycine transporter subtype 1 inhibitor, inhibited LHb activity. Collectively, these data reveal that LHb neurons are under the tonic glycine inhibition both in physiological and pathological conditions. Activation of GlyRs reverses LHb hyperactivity, alleviates aberrant behaviors, and reduces alcohol intake, thus highlighting the GlyRs in the LHb as a potential therapeutic target for alcohol-use disorders. (Li W, Zuo W, Wu W, Zuo QK, Fu R, Wu L, Zhang H, Ndukwe M, and Ye JH. Neuropharmacology. 2019 Oct; 157:107688)
Significance: This study used functional brain imaging to study the relationships between cognitive control, the severity of alcohol use disorder (AUD), and measures of negative affect such as anxiety and depression. There was greater activation in the cerebellum and temporal cortex during a cognitive interference task that was correlated with a greater degree of AUD severity and more reported negative affect. Activation in the cerebellum was still associated with negative affect after controlling for the effects of drinking history and AUD severity. These results suggest that the cerebellum may play a more prominent role in negative affect and AUD than previously realized and provides a potential target for intervention.
Impairment in cognitive control in alcohol use disorder (AUD) contributes to difficulty controlling alcohol use and, in many populations, difficulties with emotion regulation. However, the most reliable and robust marker of clinically-relevant deficits in cognitive control in AUD is unclear. Our aims were to measure relationships between BOLD signal during a Stroop task and AUD severity and change in BOLD signal and change in drinking over three weeks. We also aimed to explore the relationships between BOLD signal and subjective negative affect. Thirty-three individuals with AUD underwent a multisensory Stroop task during functional magnetic resonance imaging (fMRI), as well as a battery of neuropsychological tests and self-report assessments of negative affect and AUD severity. Greater activation in temporal gyrus and cerebellum during incongruent trials compared to congruent trials was observed, and percent signal change (incongruent minus congruent) in both clusters was positively correlated with AUD severity and self-reported negative affect. Neuropsychological task performance and self-reported impulsivity were not highly correlated with AUD severity. Hierarchical regression analyses indicated that percent signal change (incongruent minus congruent) in cerebellum was independently associated with negative affect after controlling for recent and chronic drinking. In a subset of individuals (n = 23) reduction in cerebellar percent signal change (incongruent minus congruent) was correlated with increases in percent days abstinent over 3 weeks. BOLD activation during this Stroop task may therefore be an important objective marker of AUD severity and negative affect. The potential importance of the cerebellum in emotion regulation and AUD severity is highlighted. (Wilcox CE*, Clifford J, Ling J, Mayer AR, Bigelow R, Bogenschutz MP, and Tonigan JS. Brain Imaging and Behavior 2019 May 22. doi: 10.1007/s11682-019-00126-3)
*Denotes NIAAA-funded K awardee
Significance: Lifetime alcohol drinking is often associated with anxiety, depression, and other mental health conditions such as borderline personality disorder (BPD). However, the extent to which sex differences contribute to these conditions in relation to drinking problems is not well understood. This study assessed trait anxiety, depression, and symptoms of BPD in a large sample of young adults (ages 18—30) with varying lifetime alcohol-related problems. The results showed that the correlation between trait anxiety and alcohol problems was significantly stronger in men than women, regardless of depression and BPD symptoms. These findings suggest sex-specific mechanisms underlying the relationship between trait anxiety and alcohol problems.
Objective: The co-occurrence of alcohol use disorder (AUD) and internalizing psychopathology, such as anxiety and depression, has been well documented. However, most studies of the association between alcohol problems and anxiety, do not simultaneously consider depression or borderline personality, which covary strongly with both anxiety symptoms and AUDs. The current study examined sex differences in the association between alcohol problems and anxiety, while accounting for depressive and borderline personality (BPD) symptoms. Method: A sample 810 (364 females) young adults aged 18–30 recruited from the community, who varied widely in lifetime alcohol problems, were administered diagnostic interviews and measures of a trait anxiety, depression, and BPD symptoms. Results: Analyses revealed that trait anxiety, depression, and borderline symptoms were all significantly associated with higher lifetime alcohol problems in both males and females. However, the association between trait anxiety and alcohol problems was significantly stronger for males compared with females, even when controlling for depression and BPD symptoms. There were no significant sex differences in the association between alcohol problems and symptoms of either depression or BPD symptoms. Conclusion: This suggests specific sex differences in the mechanisms by which trait anxiety is associated with alcohol problems. (Atkinson EA and Finn PR. Journal of Substance Use. 2019. 24:3, 323-328. doi: 10.1080/14659891.2019.1572800)
Significance: Effects of ghrelin administration on cortisol and aldosterone, two corticosteroid hormones involved in the neurobiology of alcohol use disorder (AUD), have been observed in previous studies. In this study, serum concentrations of cortisol and aldosterone were used to develop a model to predict the effect of ghrelin administration on alcohol craving in individuals with AUD. Intravenous ghrelin administration increased endogenous levels of cortisol and aldosterone; only the ghrelin-induced changes in aldosterone serum concentrations predicted craving. These findings provide initial evidence of a link between ghrelin and corticosteroids in the context of AUD, thereby providing additional information on how the ghrelin system may play a role in alcohol-related behaviors.
Increasing evidence supports the role of appetite-regulating hormones, including ghrelin, in alcohol use disorder (AUD). Effects of ghrelin administration on cortisol and aldosterone, two hormones known to influence the development and maintenance of AUD, have been observed in ghrelin-exposed tissues or cells, as well as rodents and healthy volunteers, however whether these effects replicate in individuals with AUD is unknown. Here, we tested the hypothesis that intravenous administration of ghrelin leads to increase in endogenous serum cortisol and aldosterone concentrations in alcohol-dependent, heavy drinking individuals, and that these changes may predict ghrelin-induced alcohol craving. This was a double-blind, placebo-controlled human laboratory study in non-treatment-seeking, heavy-drinking, alcohol-dependent individuals randomized to receive either placebo, 1 mcg/kg or 3 mcg/kg of intravenous ghrelin. Then, participants underwent a cue-reactivity procedure in a bar-like setting, which included exposure to both neutral (juice) and alcohol cues. Repeated blood samples were collected and used to measure endogenous cortisol and aldosterone serum concentrations, in response to exogenous ghrelin administration. Furthermore, cortisol and aldosterone serum concentrations were used to develop a model to predict the effect of exogenous ghrelin administration on alcohol craving. Intravenous ghrelin administration increased endogenous cortisol and aldosterone serum concentrations. While the effects on cortisol were greater than those on aldosterone, only the ghrelin-induced changes in aldosterone serum concentrations predicted craving. These findings provide initial evidence of ghrelin effects on glucocorticoids and mineralocorticoids in individuals with AUD, thereby providing additional information on the potential mechanisms by which the ghrelin system may play a role in alcohol craving and seeking in AUD. (Haass-Koffler CL, Long VM, Farokhnia M, Magill M, Kenna GA, Swift RM, and Leggio L. Neuropharmacology. 2019 Jul 13:107711. doi: 10.1016/j.neuropharm.2019.107711)
Significance: Patients who have recovered from alcoholic hepatitis (AH) remain at risk of readmission and death, outcomes generally attributed to alcohol relapse. This analysis of two different patient cohorts evaluated 30-day rates of hospital readmission, alcohol relapse, and long-term mortality in AH patients. In both cohorts, participation in early alcohol rehabilitation (within 30 days of discharge from AH treatment) was associated with decreased 30-day readmission, decreased 30-day alcohol relapse, and importantly, decreased mortality. These results suggest that all patients with AH should be formally evaluated by addiction specialists during their hospital stay and referred for treatment within 30 days of hospital discharge.
BACKGROUND & AIMS: Patients admitted to the hospital for alcoholic hepatitis (AH) are at increased risk of readmission and death. We aimed to identify factors associated with readmission, alcohol relapse, and mortality. METHODS: We performed a retrospective analysis of consecutive patients admitted with AH to a tertiary care hospital from 1999 through 2016 (test cohort, n = 135). We validated our findings in a prospective analysis of patients in a multi-center AH research consortium from 2013 through 2017 (validation cohort, n = 159). Alcohol relapse was defined as any amount of alcohol consumption within 30 days after hospital discharge. Early alcohol rehabilitation was defined as residential or outpatient addiction treatment or mutual support group participation within 30 days after hospital discharge. RESULTS: Thirty-day readmission rates were 30% in both cohorts. Alcohol relapse rates were 37% in the test and 34% in the validation cohort. Following hospital discharge, 27 patients (20%) in the test cohort and 19 patients (16%) in the validation cohort attended early alcohol rehabilitation. There were 53 deaths (39%) in a median follow-up time of 2.8 years and 42 deaths (26%) in a median follow-up time of 1.3 years, respectively. In the test cohort, early alcohol rehabilitation reduced odds for 30-day readmission (adjusted odds ratios [AOR] 0.16; 95% CI, 0.04-0.65; P = .01), 30-day alcohol relapse (AOR, 0.11; 95% CI, 0.02-0.53; P < .001), and death (adjusted hazard ratio [AHR], 0.20; 95% CI, 0.05-0.56; P = .001). In the validation cohort early alcohol rehabilitation reduced odds for 30-day readmission (AOR, 0.30; 95% CI, 0.09-0.98; P = .04), 30-day alcohol relapse (AOR 0.09; 95% CI, 0.01-0.73; P = .02), and death (AHR, 0.20; 95% CI, 0.01-0.94; P = .04). A model combining alcohol rehabilitation and bilirubin identified patients with readmission to the hospital within 30 days with an area under the receiver operating characteristic curve of 0.73. CONCLUSIONS: In an analysis from two cohorts of patients admitted with AH, early alcohol rehabilitation can reduce risk of hospital readmission, alcohol relapse, and death and should be considered as a quality indicator in AH hospitalization treatment. (Peeraphatdit TB, Kamath PS, Karpyak VM, Davis B, Desai V, Liangpunsakul S, Sanyal A, Chalasani N, Shah VH, and Simonetto DA. Clin Gastroenterol Hepatol. 2019 Apr 28. pii: S1542-3565(19)30438-0)
Health Care Use Over 3 Years After Adolescent SBIRT
Significance: Research suggests that screening, brief intervention, and referral to treatment (SBIRT) in pediatric primary care may improve patient outcomes, but few studies have examined its effects on health care use or the development of medical or mental health comorbidities over time. This study used electronic health data to examine subsequent health care use among adolescents from a randomized clinical trial comparing usual care to two modalities of delivering SBIRT in pediatric primary care (either pediatrician- or behavioral clinician-delivered). Results indicated that patients with access to SBIRT had fewer comorbidities, fewer psychiatry visits at 1 year, and fewer substance use diagnoses, as well as lower outpatient use over 3 years. These findings suggest that providing SBIRT in primary care may reduce health care use and improve adolescent health.
BACKGROUND: Most studies on adolescent screening, brief intervention, and referral to treatment (SBIRT) have examined substance use outcomes. However, it may also impact service use and comorbidity-an understudied topic. We address this gap by examining effects of SBIRT on health care use and comorbidities. METHODS: In a randomized trial sample, we assessed 3 SBIRT care modalities: (1) pediatrician-delivered, (2) behavioral clinician-delivered, and (3) usual. Medical comorbidity and health care use were compared between a brief-intervention group with access to SBIRT for behavioral health (combined pediatrician and behavioral clinician arms) and a group without (usual care) over 1 and 3 years. RESULTS: Among a sample of eligible adolescents (n = 1871), the SBIRT group had fewer psychiatry visits at 1 year (incidence rate ratio [iRR] = 0.76; P = .05) and 3 years (iRR = 0.65; P < .05). Total outpatient visits did not differ in year 1. The SBIRT group was less likely to have mental health diagnoses (odds ratio [OR] = 0.69; 95% confidence interval [CI] = 0.48-1.01) or chronic conditions (OR = 0.66; 95% CI = 0.45-0.98) at 1 year compared with those in usual care. At 3 years, the SBIRT group had fewer total outpatient visits (iRR = 0.85; P < .05) and was less likely to have substance use diagnoses (OR = 0.64; 95% CI = 0.45-0.91) and more likely to have substance use treatment visits (iRR = 2.04; P < .01). CONCLUSIONS: Providing SBIRT in pediatric primary care may improve health care use and health, mental health, and substance use outcomes. We recommend further exploring the effects of SBIRT on these outcomes. (Sterling S, Kline-Simon AH, Jones A, Hartman L, Saba K, Weisner C, and Parthasarathy S. Pediatrics. 2019 May;143(5). pii: e20182803. doi: 10.1542/peds.2018-2803)
Significance: “Secondhand effects” of alcohol refer to harms resulting from others’ drinking. This study examined the prevalence of alcohol’s secondhand effects and whether the prevalence of these effects differed based on the strength of a state’s policies (expressed as an Alcohol Policy Scale value). Secondhand harms in three categories – aggression-related, family- or financial-related, and driving-related – were experienced by 16.8 percent of people under age 40 and 7.8 percent of people over age 40. For those under 40, state policies known to reduce binge drinking and impaired driving were linked to lower levels of reported aggression-related harms and drunk driving-related harms. These findings demonstrate that many people suffer consequences from alcohol use by others and suggest that state policies known to reduce binge drinking and impaired driving might also reduce the secondhand harms of alcohol, particularly among individuals under 40.
BACKGROUND: Although restrictive state alcohol policy environments are protective for individuals' binge drinking, research is sparse on the effect of alcohol policies on alcohol's harms to others (AHTO). We examined the lagged associations between efficacy of U.S. state alcohol policies and number of harms from others' drinking 1 year later. METHODS: Individuals with AHTO data in a nationally representative sample of U.S. adults (analytic sample n = 26,744) that pooled the 2000, 2005, 2010, and 2015 National Alcohol Surveys and a 2015 National Alcohol's Harm to Others Survey were linked with prior-year state policy measures. We used 2 measures from the Alcohol Policy Scale (APS)-effectiveness in reducing (i) binge drinking and (ii) impaired driving, based on experts' efficacy judgments regarding 29 state alcohol policies. Three 12-month AHTO measures (due to another drinker) were experiencing: (i) either family/marriage difficulties or financial troubles; (ii) being assaulted or vandalized; and (iii) passenger with drunk driver or traffic accident. Multilevel models accounting for clustering within states and stratified by age-groups (<40 vs. ≥40) examined associations between the APS and AHTO measures, controlling for individual covariates (gender, race, education, employment and marital status, family problem-drinking history) of the victim. RESULTS: Only for those aged <40, the lagged APS-Binge drinking and APS-Impaired driving scores were each inversely associated with aggression-related harms and, separately, with drunk driving-related harm from someone else's drinking (ps < 0.05 to < 0.01). Family/financial harms were not associated with APS scores for either age-group. Composite AHTO measures (any of 3 harm-types) also were inversely associated with stronger state alcohol policy environments (ps < 0.05 to <0.01). CONCLUSIONS: State alcohol policies may be effective in reducing, to a meaningful degree, aggression-related harms and vehicular hazards due to other drinkers, but mainly in those under 40. (Greenfield TK, Cook WK, Karriker-Jaffe KJ, Patterson D, Kerr WC, Xuan Z, and Naimi TS. Alcohol Clin Exp Res. 2019 Jun;43(6):1234-1243. doi: 10.1111/acer.14054)
NIAAA COMMUNICATIONS ACTIVITIES
Press and Publications Activities:
Recent News Media Interviews: Dr. Koob continues to speak with a variety of national and international news outlets on timely topics related to NIAAA’s research and its impact on treatment and prevention of alcohol misuse and AUD. Notable interviews by Dr. Koob and other staff since April 2019 include New York Times, Boston Globe, CNN en Español, The Guardian, NPR, Philadelphia Inquirer, and The Washington Post.
Press Releases:
- Dr. Carlo C. DiClemente to Deliver 11th Annual Jack Mendelson Honorary Lecture at the National Institutes of Health (July 9, 2019)
- Integrated stepped alcohol treatment for people in HIV care improves both HIV and alcohol outcomes (May 17, 2019)
- NIAAA Honors Dr. Geoffrey K. Mumford with Senator Harold Hughes Award (May 14, 2019)
Please see the News and Events section of the NIAAA website for this and other news releases.
Publication Statistics: In the month of July 2019, NIAAA filled orders for 15,181 copies of print publications. As of July 17, 2019, there were 30,045 Granicus/GovDelivery listserv subscribers to Alcohol Research: Current Reviews; 23,779 to the NIAAA Spectrum; 893 to News Alerts; and 22,877 to receive general information. 
Social Media Highlights:
- In recent months, NIAAA has been spotlighting summer students in its ongoing #NIAAAtraining series, which focuses on training opportunities and the experience of trainees at the institute.
- Summer safety has also been featured on social media, with messages about the risks of mixing alcohol with swimming and boating, the increased risk of sunburn while drinking, and the dangers of dehydration from alcohol.
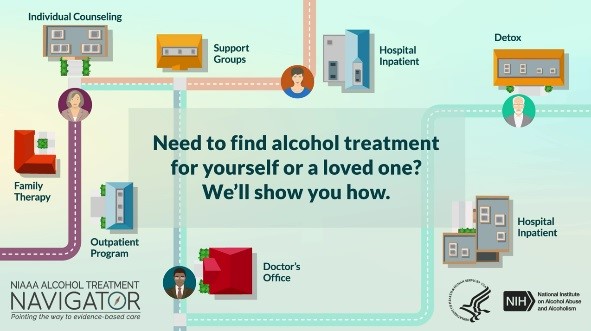
- NIAAA continues to use social media to promote the Alcohol Treatment Navigator and recently released a new animation about the resource. NIAAA’s social media audience is growing steadily with 23,600 Twitter followers and 800 followers on its Instagram account.
Partnerships, Outreach and Public Liaison Activities:
Summer Safety Outreach
NIAAA disseminated its fact sheet titled “Risky Drinking Can Put a Chill on Your Summer Fun” to the media through PR Newswire’s US1 distribution with AP photo release on June 6 and July 3, 2019. The fact sheet was posted by Internet news outlets such as The Daily Meal, WBBH-TV, One News Page, News Blaze, The Street, KWTV-TV, and Buffalo News as well as business journals, industry publications, and numerous major television network (FOX, NBC, CBS, ABC) local affiliates nationwide. The release had a total of 164 unique links, representing a total potential audience of 71 million people. The fact sheet graphic also appeared on Cision’s Times Square billboard a total of 21 times on June 6, and 11 times on July 3, 2019. In addition to the PR Newswire releases, four Cision email blasts were distributed on May 29, June 12 and 25, and July 10 to a total of 17,360 TV and print reporters. Health News Digest, Lansing State Journal, News-Star.com, and NewKerala.com ran related articles after receiving the Cision emails.
Overdose Fact Sheet – A focused and targeted summer promotion of the NIAAA fact sheet titled “Alcohol Overdose: The Dangers of Drinking Too Much” resulted in a 174 percent increase in pageviews compared to the same period in 2018.
High School Graduation – The NIAAA fact sheet titled “Parents—Talk With Your High School Grads About Celebrating Safely” was disseminated to the media through PR Newswire on US1 distribution with AP photo release on May 13 and May 15, 2019. The fact sheet was posted by Internet news outlets such as Ask.com, Sun Coast News Network, Rockford Register Star, Washington, DC CityRoom, as well as blogs, business journals, industry publications, and numerous major television network (FOX, NBC, CBS, ABC) local affiliates nationwide. The release had a total of 147 unique links, representing a total potential audience of 49 million people. The fact sheet graphic also appeared on Cision’s Times Square billboard a total of 10 times on May 13, 2019, and five times on May 15, 2019. In addition to the PR Newswire releases, a Cision email blast was sent to more than 2,100 local and national TV and print reporters on May 20. NBC29.com, CBS19.com, Motherhood Moment, News-Star.com, and NewKerala.com ran related stories from information in the Cision email.
Back to College – The NIAAA fact sheet titled “Fall Semester–A Time for Parents to Discuss the Risks of College Drinking” was disseminated to the media through Cision/PR Newswire’s US1 distribution with AP photo release on August 13 and 19. Pickup is being monitored.
Select Partnership Updates 
- NABCA Webinar: During Alcohol Awareness Month, Dr. Aaron White presented a webinar on April 10 with the National Alcohol Beverage Control Association (NABCA). The title was “Changes in Alcohol Use in the US – ED Visits and Other Outcomes.” The presentation is available at https://youtu.be/yA-pPJr2aW0.
- SADD: During National Prevention Week, May 13—17, in partnership with NIAAA, the group Students Against Destructive Decisions (SADD) issued a video challenge, calling on student members to submit brief videos with messages that counter misconceptions about alcohol and addressed students’ concerns about alcohol misuse. More than 30 student entries were received. Selected participating SADD organizations were awarded a stipend from NIAAA to attend SADD’s National Conference on June 23-25. SADD showcased the videos on its social media platform and at multiple conference events.
- CADCA: On July 17, Dr. Ralph Hingson presented at the Community Anti-Drug Coalitions of America (CADCA) Mid-Year Training Institute. He spoke on “New Research Since the Surgeon General's Call to Action to Prevent and Reduce Underage Drinking.”
Special Events
- Hughes Award:
 On May 14, NIAAA presented the Senator Harold Hughes Memorial Award to Dr. Geoffrey K. Mumford, Associate Executive Director for Government Relations in the Science Directorate of the American Psychological Association (APA). The Hughes Award recognizes the contributions of an individual whose work translates research into practice, and builds bridges across the alcohol prevention, treatment and policy-making communities. The award is named for Harold Hughes, a former Iowa Governor and U.S. Senator, who was a major force behind the 1970 legislation that led to the creation of NIAAA.
On May 14, NIAAA presented the Senator Harold Hughes Memorial Award to Dr. Geoffrey K. Mumford, Associate Executive Director for Government Relations in the Science Directorate of the American Psychological Association (APA). The Hughes Award recognizes the contributions of an individual whose work translates research into practice, and builds bridges across the alcohol prevention, treatment and policy-making communities. The award is named for Harold Hughes, a former Iowa Governor and U.S. Senator, who was a major force behind the 1970 legislation that led to the creation of NIAAA. - Mendelson Lecture:
 On July 11, 2019, Dr. Carlo C. DiClemente, Professor Emeritus, Department of Psychology, University of Maryland, Baltimore County, presented the 11th Annual Mendelson Lecture, “Is Relapse and Recycling Necessary for Recovery from Alcohol Use Disorder?” NIAAA established the lecture series as a tribute to Dr. Jack Mendelson, who made remarkable contributions to the field of clinical alcohol research. A video recording of Dr. DiClemente’s lecture is available at https://videocast.nih.gov/summary.asp?live=33218&bhcp=1.
On July 11, 2019, Dr. Carlo C. DiClemente, Professor Emeritus, Department of Psychology, University of Maryland, Baltimore County, presented the 11th Annual Mendelson Lecture, “Is Relapse and Recycling Necessary for Recovery from Alcohol Use Disorder?” NIAAA established the lecture series as a tribute to Dr. Jack Mendelson, who made remarkable contributions to the field of clinical alcohol research. A video recording of Dr. DiClemente’s lecture is available at https://videocast.nih.gov/summary.asp?live=33218&bhcp=1.
Web Activities
- The Communication and Public Liaison Branch (CPLB) Launches New Customer Satisfaction Survey: CPLB’s web team added a new customer satisfaction survey to the NIAAA Main website and the online Alcohol Treatment Navigator. CPLB has collected more than 2,000 responses for NIAAA Main (4 weeks’ worth of data). These measures will provide useful data on what our web visitors are looking for and how we can improve our sites.
- Grantees Offer Feedback on NIAAA Website: As part of a long-term redesign project, CPLB reached out to NIAAA grantees for feedback about our website (what they use it for and how we can improve it). Dozens of grantees responded. This feedback will help CPLB’s web team determine continued improvements in web content, organization, and design during our Drupal 8 software migration.
- CPLB Implements Web Upgrades: in recent months CPLB has—
- Enhanced many of NIAAA’s popular web publications, brochures, and fact sheets by improving usability through responsive designs tailored to mobile devices.
- Redesigned the publications web order form onto NIAAA’s main web platform. (See https://www.niaaa.nih.gov/niaaa-publications-order-form)
- Implemented responsive design and other search engine optimization (SEO) methods.

