Goal 4: Improve Diagnosis and Expand Treatment of Alcohol Use Disorder and Alcohol-Related Conditions
NIAAA’s Long-Term Vision
To develop effective treatments that are accessible to every person with an alcohol-related health problem.
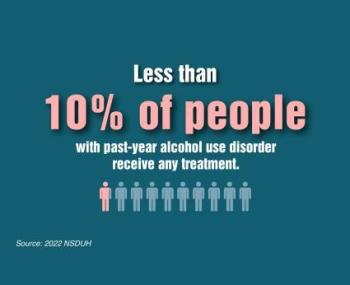
Alcohol-related health conditions are currently underdiagnosed and undertreated. Less than 10% of people with alcohol use disorder (AUD) receive any help despite the availability of evidence-based pharmacological and behavioral treatments.1 In addition, there are no U.S. Food and Drug Administration (FDA)-approved medications for alcohol-associated liver disease (ALD), and evidence-based treatment strategies are also needed for other alcohol-associated conditions, such as fetal alcohol spectrum disorders (FASD). Developing, optimizing, and implementing evidence-based treatment strategies for AUD and alcohol-related conditions remain high priorities for NIAAA. Likewise, research to improve the early identification and diagnosis of alcohol-related health issues to enhance treatment effectiveness are also important NIAAA priorities.
As described under the Cross-Cutting Theme on Integrating care for alcohol-related problems, AUD commonly co-occurs with other health conditions, including organ and tissue damage and mental health conditions. Integrating treatment for AUD with treatment of co-occurring conditions related directly or indirectly to alcohol use is an important step toward improving alcohol-related outcomes and overall health.
Moreover, improved diagnostic techniques for FASD would enable more accurate diagnosis and earlier intervention, offering a better chance for improved outcomes. The Cross-Cutting Research Program on Fetal Alcohol Spectrum Disorders explores this research area.
Goal 4 research topics are integrally linked to the Cross-Cutting Research Themes. Examples of NIAAA research priorities in this area include the following objectives.
1SAMHSA, Center for Behavioral Health Statistics and Quality. 2022 National Survey on Drug Use and Health. Table 5.32B— Received substance use treatment in past year: among people aged 12 or older; by age group and past year drug use disorder, past year alcohol use disorder, past year drug and alcohol use disorder, and past year substance use disorder, percentages, 2021 and 2022. [cited 2023 Dec 13]. Available from: https://www.samhsa.gov/data/sites/default/files/reports/rpt42728/NSDUHDetailedTabs2022/NSDUHDetailedTabs2022/NSDUHDetTabsSect5pe2022.htm?s=5.32&#tab5.32b