Women and Alcohol

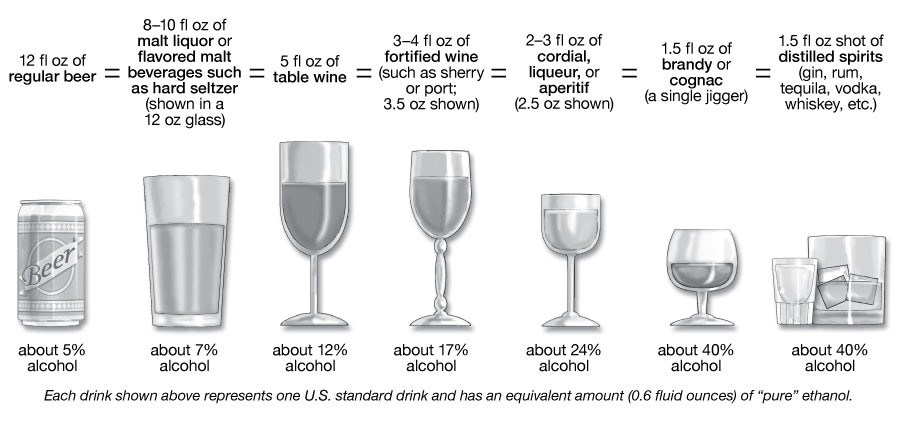
Research shows that alcohol use and misuse among women are increasing.1,2 While alcohol misuse by anyone presents serious public health concerns, women who drink have a higher risk of certain alcohol-related problems compared to men.3 It is important for women to be aware of these health risks and of the 2020–2025 Dietary Guidelines for Americans so that they can make informed decisions about alcohol use. Adult women of legal drinking age can choose to not drink or to limit their intake to one drink or less in a day, when alcohol is consumed.4 This amount is not intended as an average but rather as a daily limit. Alcohol-related risks may be minimized, though not eliminated, by limiting intake. Some individuals should avoid alcohol completely, such as women who are pregnant or might be pregnant.4
Why Do Women Face Higher Risks?
Studies show that women start to have alcohol-related problems sooner and at lower drinking amounts than men and for multiple reasons.3 On average, women weigh less than men. Also, alcohol resides predominantly in body water, and pound for pound, women have less water in their bodies than men. This means that after a woman and a man of the same weight drink the same amount of alcohol, the woman’s blood alcohol concentration (the amount of alcohol in the blood) will tend to be higher, putting her at greater risk for harm. For example, research suggests that women are more likely than men to experience hangovers and alcohol-induced blackouts at comparable doses of alcohol.5,6 Other biological differences may contribute as well.
What Are the Health Risks?
Medical Emergencies and Deaths
Women, compared to men, have had larger increases in alcohol-related emergency department visits, hospitalizations, and deaths in the past 20 years.7
Alcohol Use Disorder
Alcohol use disorder (AUD) is characterized by an impaired ability to stop or control alcohol use despite adverse social, occupational, or health consequences. It is a spectrum disorder and can be mild, moderate, or severe, and it encompasses the conditions that some people refer to as alcohol abuse, alcohol dependence, or the colloquial term alcoholism. (To be diagnosed with AUD, a person must meet certain diagnostic criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition.) AUD can cause lasting changes in the brain that make people vulnerable to relapse. Women are less likely than men to receive treatment for AUD.8
Liver Damage
Women who regularly misuse alcohol are more likely to develop alcohol-associated hepatitis, a potentially fatal alcohol-related liver condition, than men who drink the same amount.9 This pattern of drinking can also lead to cirrhosis (permanent liver scarring).
Heart Disease
Long-term alcohol misuse is a leading cause of heart disease. Women are more susceptible to alcohol-related heart disease than men, even though they may consume less alcohol over their lifetime than men.3
Brain Damage
Research suggests that alcohol misuse produces brain damage more quickly in women than in men.10 In addition, a growing body of evidence shows that alcohol can disrupt normal brain development during the adolescent years, and there may be differences in the impact of alcohol on the brains of teenagers who drink.11 For example, in one study, teen girls who reported binge drinking, but not teen boys who reported binge drinking, showed less brain activity and worse performance on a memory test than peers who drank lightly or abstained.12 Similarly, teen girls who drank heavily showed a greater reduction in the size of important brain areas involved in memory and decision-making than teen boys who engaged in heavy drinking.13 Women also may be more susceptible than men to alcohol-related blackouts, which are gaps in a person’s memory for events that occurred while they were intoxicated. These gaps happen when a person drinks enough alcohol to temporarily block the transfer of memories from short-term to long-term storage—known as memory consolidation—in a brain area called the hippocampus.6

Breast Cancer
Research has shown an important association between alcohol consumption and breast cancer—even one drink per day can increase a woman's risk for breast cancer by 5% to 15% compared to women who do not drink at all.14–16
Alcohol and Pregnancy
There is no known safe amount of alcohol consumption for women who are pregnant or might become pregnant. Prenatal alcohol exposure can cause children to experience physical, cognitive, and behavioral problems, any of which can be components of fetal alcohol spectrum disorders. Drinking during pregnancy can also increase the risk for preterm labor.
Some Women Should Avoid Alcohol Entirely
According to the 2020–2025 Dietary Guidelines for Americans, it is safest to avoid alcohol altogether if you:
- Are taking medications that interact with alcohol
- Are managing a medical condition that can be made worse by drinking
- Are under the age of 21, the minimum legal drinking age in the United States
- Are recovering from AUD or unable to control the amount you drink
- Are pregnant or might be pregnant
In addition, certain individuals should avoid alcohol completely, particularly those who experience facial flushing and dizziness when drinking alcohol. Also in this category are older adults, anyone planning to drive a vehicle or operate machinery, and individuals who participate in activities that require skill, coordination, and alertness.
To see whether your pattern of alcohol use puts you at risk for AUD, please visit Rethinking Drinking at: rethinkingdrinking.niaaa.nih.gov
1. White A, Castle IJP, Chen CM, Shirley M, Roach D, Hingson R. Converging patterns of alcohol use and related outcomes among females and males in the United States, 2002 to 2012. Alcohol Clin Exp Res. 2015;39:1712–26. PubMed PMID: 26331879
2. Slade T, Chapman C, Swift W, Keyes K, Tonks Z, Teesson M. Birth cohort trends in the global epidemiology of alcohol use and alcohol-related harms in men and women: systematic review and metaregression. BMJ Open. 2016;6(10):e011827. PubMed PMID: 27797998
3. Erol A, Karpyak V. Sex and gender-related differences in alcohol use and its consequences: contemporary knowledge and future research considerations. Drug and Alcohol Dependence. 2015;156:1–13. PubMed PMID: 26371405
4. U.S. Department of Health and Human Services (HHS), U.S. Department of Agriculture (USDA). Dietary guidelines for Americans, 2020–2025. 9th ed. Washington: HHS and USDA; 2020 [cited 2022 Jul 13]. Alcoholic beverages; p. 49. Available from: https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf
5. Vatsalya V, Stangl BL, Schmidt VY, Ramchandani, VA. Characterization of hangover following intravenous alcohol exposure in social drinkers: methodological and clinical implications. Addict Biol. 2018;23(1):493–502. PubMed PMID: 27860050
6. Hingson R, Zha W, Simons-Morton B, and White A. Alcohol-induced blackouts as predictors of other drinking related harms among emerging young adults. Alcohol Clin Exp Res. 2016;40(4):776–84. PubMed PMID: 27012148
7. White AM. Gender differences in the epidemiology of alcohol use and related harms in the United States. Alcohol Res. 2020;40(2):01. PubMed PMID: 33133878
8. Gilbert PA, Pro G, Zemore SE, Mulia N, Brown G. Gender differences in use of alcohol treatment services and reasons for nonuse in a national sample. Alcohol Clin Exp Res 2019;43(4)722–31. PubMed PMID: 30807660
9. Guy J, Peters MG. Liver disease in women: the influence of gender on epidemiology, natural history, and patient outcomes. Gastroenterol Hepatol. 2013;9(10):633–639. PubMed PMID: 24764777
10. Hommer DW. Male and female sensitivity to alcohol-induced brain damage. Alcohol Res Health. 2003;27(2):181–5. PubMed PMID: 15303629
11. Jones SA, Lueras JM, Nagel BJ. Effects of binge drinking on the developing brain. Alcohol Res. 2018;39(1): 87–96. PubMed PMID: 30557151
12. Squeglia LM, Schweinsburg AD.,Pulido C, Tapert SF. Adolescent binge drinking linked to abnormal spatial working memory brain activation: differential gender effects. Alcohol Clin Exp Res 2011;35(10):1831–41. PubMed PMID: 21762178
13. Seo S, Beck A, Matthis C, Genauck A, Banaschewski T, Bokde ALW, Bromberg U, Büchel C, Quinlan EB, Flor H, Frouin V, Garavan H, Gowland P, Ittermann B, Martinot JL, Paillère Martinot ML, Nees F, Papadopoulos Orfanos D, Poustka L, Hohmann S, Fröhner JH, Smolka MN, Walter H, Whelan R, Des rivières S, Heinz A, Schumann G, Obermayer K. Risk profiles for heavy drinking in adolescence: differential effects of gender. Addict Biol. 2019;24(4):787–801. PubMed PMID: 29847018
14. Choi YJ, Myung SK, Lee JH. Light Alcohol Drinking and Risk of Cancer: A Meta-Analysis of Cohort Studies. Cancer Res Treat. 2018 Apr;50(2):474-487. doi: 10.4143/crt.2017.094. Epub 2017 May 22. PubMed PMID: 28546524
15. Bagnardi V, Rota M, Botteri E, Tramacere I, Islami F, Fedirko V, Scotti L, Jenab M, Turati F, Pasquali E, Pelucchi C, Galeone C, Bellocco R, Negri E, Corrao G, Boffetta P, La Vecchia C. Alcohol consumption and site-specific cancer risk: a comprehensive dose-response meta-analysis. Br J Cancer. 2015 Feb 3;112(3):580-93. doi: 10.1038/bjc.2014.579. Epub 2014 Nov 25. PubMed PMID: 25422909
16. Cao Y, Willett WC, Rimm EB, Stampfer MJ, Giovannucci EL. Light to moderate intake of alcohol, drinking patterns, and risk of cancer: results from two prospective US cohort studies. BMJ. 2015 Aug 18;351:h4238. doi: 10.1136/bmj.h4238. PubMed PMID: 26286216